Giving a patient medications in the ER, having them pop positive on a test, and then withholding further medications because…
Monday Morning Update 6/27/11
Google makes it official: the company is shutting down three-year-old Google Health on January 1, 2012. Google predictably did what its know-it-all technology company predecessors have done over the years: dipped an arrogant and half-assed toe into the health IT waters; roused a loud rabble of shrieking fanboy bloggers and reporters (many of them as light on healthcare IT experience as Google) who instantly declared it to be the Second Coming that would make all decades-old boring vendors instantly obsolete or subservient to the Googleplex; and then turned tailed and slunk off at the first sign of lackluster ROI, leaving the few patients and providers who actually cared high and dry except for those same old boring vendors who have stuck it out for decades instead of chasing whatever sector looked juicy at the moment.
Why did Google Health fail? Simple and obvious: consumer demand for personal health records is close to zero, which has always been the case and probably always will be. Convincing patients to take the time and effort to maintain PHRs is as tough a sell as convincing doctors to voluntarily use CPOE, and for the same reasons: those doing the work don’t get much benefit. Patients don’t want to maintain their own records and clinicians aren’t about to trust patient-maintained information for making treatment decisions (not to mention that taxpayer-incented HIEs and Epic’s MyChart are stealing their thunder by not relying on patient-powered sneakernet in the first place). PHRs aren’t fun. They don’t accrue Farmville points, you can’t put pictures of your cat or a funny YouTube video on them, and you don’t get HITECH money for typing in your weight every now and then. The only model Google knows involves near-universal adoption that gets advertisers salivating, not having a tiny contingent of wellness buffs and savvy chronic disease suffers using their free online service. Ultimately, Google’s problem is that an awful lot of Americans care about reality TV and celebrity gossip more than their health. They’re more interested in patch-me-up-doc “healthcare” than I-need-to-make-better-choices “health” that requires proactive electronic tools. The most shocking aspect of Google Health’s announcement in 2008 was either that Google hadn’t figured that out or that they thought they could succeed anyway.
Want to bet that Google will come crawling back to healthcare one of these days when earnings start to slip? That’s what generally happens with those short attention span technology vendors. Like Microsoft before it, Google has gone from a dominant force that can do no wrong to a clearly fallible company that makes a ton of money, but that often is more of a follower than a leader with surprisingly routine and easily predicted product failures. And speaking of Microsoft, I’m not sure whether Google Health’s timely death is good news or bad for HealthVault, a better product, but still facing the same uninterested market even with the loss of its only high-profile competitor (advantage: Dossia?)
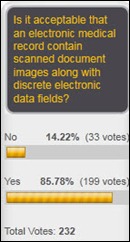
It’s OK to include scanned documents in an EMR, say 86% of respondents, while a less-forgiving 14% of purists say no way, electronic doesn’t just mean electronic, it means discrete data only. New poll to your right, in honor of the dearly departed Google Health: do you keep a current and medical reliable electronic Personal Health Record? I asked that same question in 2007, when 88% of the most technologically and medically savvy people in healthcare said they did not (maybe Google should have taken those results as one of those warning cow skulls in the desert).
Suggestion to anyone claiming to be an insightful Epic expert: your credibility will be enhanced if you spell the company’s name right (it is not EPIC).
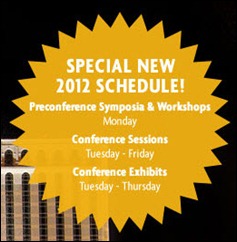
A company approached me about sponsoring the HIStalk reception at HIMSS next year (I love that I don’t have to troll to get companies interested since I don’t have the time or inclination to do that). I found out from those folks something I hadn’t noticed: HIMSS has completely screwed around with the Las Vegas conference days, with the pre-conference stuff starting on Monday (Saturday is now Monday, in other words) and the sessions run Tuesday through Friday (so everybody will need to bail out for home on Thursday instead of Wednesday). Great – now you can’t do a Saturday night stay when trying to find a cheap flight and we’ll either have to travel with all the other business schmos on Monday or fly out a day early. They’ve moved my cheese and I’m unhappy, but I’ll get over it. So, despite my concluding HISsies slide from Orlando, the reception is probably not going to be Monday night if I decide to do another one. If you’re slotted to present a Friday session, you might want to plan for a roundtable instead of an auditorium.
I am absolutely loving Vince Ciotti’s HIStory series. He’s getting lots of e-mails and kudos, even from 20-something HIT sprouts who understand the “doomed to repeat history” thing and figure they can learn from the pioneer diaries. Vince recently had calls from Jim Pesce (McAuto) and Mike Kaufman, who are following his series and contributed to the installment above (I’m really impressed with Mike’s history since I didn’t realize his deep roots when he and I have exchanged e-mails over the years). E-mail Vince if you have some history inside your head or on paper that would round out his recollections. The industry goes back to the late 1960s (Meditech was formed in 1969), so with 40-plus years having gone by, it’s time to document some of this stuff.
Speaking of Mike Kaufman, in Googling to see what he’s up to, I see that he, along with fellow former Eclipsys SVP Hans Boerma MD and money guy Frank Panaccio formed KBT Partners, which offers advisory services to healthcare IT and related companies.

I’m also quite enjoying the work of Micky Tripathi in his monthly Pretzel Logic column on HIStalk Practice. His writing is fluid and personal (not to mention entertaining) and he’s obviously an expert in all things EMR (fortunately, since he’s the president and CEO of the Massachusetts eHealth Collaborative). I just posted his Quality Measures Conundrum piece and it should be required reading for anybody who cares about EMRs or Meaningful Use.
My Time Capsule editorial this week from 2006: Medical Equipment Sales Boom While Health IT Struggles. A snip: “The takeaway message is that, science aside, doctors and hospitals will utilize the hell out of something when they’re paid to do so (equipment, drugs, supplies, and for-profit referral centers). While it’s nice if patient care is improved, it’s only mandatory that it not be worsened.”
A Harvard Business Review working paper covers why creative tension among company executives can be a good thing. One of its examples is Misys CEO Mike Lawrie, who in 2008 insisted that the company’s open source division not be rolled into Allscripts but rather allowed to compete with it for resources, which supposedly benefited both groups.
Speaking of Misys, the company offering to buy it is revealed as Fidelity National Information Services, a Jacksonville, FL-based bank technology firm that has a healthcare division (benefit administration, PHR, consumer health portal, ID cards, lockbox, revenue cycle).
Weird News Andy revives this story: mourners filing past the coffin at a Russian woman’s funeral are startled when she raises up and begins screaming, not nearly as dead as the local hospital had said. The funeral-goers’ time wasn’t wasted, however: the woman had a heart attack from all the commotion and died minutes later in the same hospital.
A survey finds that no surveyed physicians in the UK, New Zealand, Canada, and Sweden said they practice defensive medicine, compared to the 92% in the US who admit to letting fear of lawsuits drive their medical decisions.
CapSite releases the Lite version of its database, strictly for providers and hospitals. The Web-based tool provides access to thousands of contracts and proposals from peer institutions, complete with pricing and T&C covering 800 vendors in HIT, imaging, medical devices, and services. It’s free for 30 days and the company is signing me up to check it out, so I’ll be interested to snoop around since I love looking at contracts.
Athenahealth buys Point Lookout Resort and Conference Center, 396-acre, $7.7 million property near its Belfast, Maine operations center, which it will use for client and employee training. The facility overlooks Penobscot Bay and has 106 cottages, a bowling alley, and a beach. I’m thinking we need an HIT geek summer camp, complete with marshmallow roasts, snipe hunts, and furtive ukelele-inspired groping around the campfire.
OptumInsight (formerly Ingenix) is awarded a patent for its LifeCode natural language processing technology, which can extract content and context from electronic medical records. That technology runs the company’s computer-assisted coding applications, which the company says can ease the transition to ICD-10.
I’m pleased with this find since I’m thrifty (cheap, some might say, including someone with whom I share a bed). I take low-dose lisinopril for blood pressure (my BP is only 115/55, but my doc likes me to take it for some reason). I thought Walgreens offered $4 generics, but they don’t any more, so they charged me $10 for 30 tablets. I looked for alternatives and found that not only does Walmart offer a long list of maintenance meds for $10 for a 90-day supply, but mail delivery to your door is free. That is Walgreens Strike 2, the first being that they charge almost $50 for a vial of Canine HIStalk’s insulin while Walmart sells their custom-relabeled Novo Nordisk insulin for only $24.88. We may have a healthcare crisis in this country, but it would be a heck of a lot worse without Walmart (at least now that they offer health insurance to more of their employees).
Atlanta-based startup Digital Assent, which developed the PatientPad ad-powered patient check-in tool for practices, raises $7.5 million in a Series B funding round. The founders came from Sythis, which developed an interactive selling solution that licensed its technology for PatientPad.
Sad: a hospital-based physician finds that someone is checking out porn and Googling phrases such as “rat poison symptoms in humans” on his office computer. It turns out to be the hospital’s night shift security guard, who has since confessed to trying to kill his family by poisoning them and who is now charged with beating his pregnant wife, his father-in-law, and his five-year-old daughter to death with a baseball bat and then burning down his house.
Cleveland’s MetroHealth System, getting heat from the county council about no-bid consulting contracts and excessive spending, takes positive action: it hires a $300 per hour PR company (without bidding, I assume) to help its executives practice for their appearance in front of the investigating committee.
Another Weird News Andy story that has me in stitches is this story, which he entitles Four Inches? Just a Flesh Wound. An 11-year-old girl trimming her horse’s mane opens up a 10 cm gash in her chest when the horse bolts. Her mother calls emergency response for an ambulance, only to be told to clean the wound, apply pressure, give aspirin, and then drive to the nearest hospital within eight hours or so. The hospital’s first question when she arrived: “Why didn’t you call an ambulance?”





Wow – I really appreciated your take on Google health and about the technology industry’s approach to healthcare in general. You could not have been more spot-on – especially the fact that physicians have no regard (nor time) for PHRs whatsoever and that people get no intrinsic reward for maintaining one. Another fallacy of applications pushers even within our industry is that physicians will take time during an encounter to toggle to another application to get additional insight or data. So many new “applications” really need to be built as modules within the EMRs and other tools we already heave so that their value is delivered as part of an integrated tool. Great as always.
The comment about “EPIC” experts reminded me of something.
After judy’s talk to her company to refer to it as “Epic” for branding purposes. I believe the logic was that no major brand is two words (Epic Systems) using apple, google, microsoft as examples I purposely try to remember and refer to it as Epic Systems whenever possible.
I wonder if GT.M will make more inroads if that FIS MISYS deal goes through. Does anyone know if the old Allscripts and Sunquest systems are “married” to Cache yet? FIS would do well to revert back to the MUMPS standard and move everything in-house by porting it to GT.M.
I found your statement revealing of your incredible insight: “Convincing patients to take the time and effort to maintain PHRs is as tough a sell as convincing doctors to voluntarily use CPOE, and for the same reasons: those doing the work don’t get much benefit. ”
I would like to take this opportunity to tweak the concept. There is not much interest for PHRs, but, with CPOE, it is that there are signs of harm, requiring 24/7 vigilance to protect. CPOE is also an impediment to safe and efficetive communication. You know all about the usability issues, or lack thereof.
Sincerely,
Ino
What a coincidence – the comments to the news about Google Health’s demise carries Microsoft as the “HIStalk Featured Sponsor” 🙂
What surprised me about the development of Google Health was the Microsoft-like disdain towards existing standards. Given the necessity to automate the input and output of healthcare data in a PHR, Google did not make any effort to participate in HL7 or IHE activities, or to support any of these standards and specifications. Actually, Microsoft have shown more support (at least until recently) for standards than Google in the healthcare area, which is usually reversed.
Don’t celebrate too long about Google giving up on Google Health.
It was also announced that one of the ONCHIT tiger groups has accepted the PCAST recommendation that the one of the solutions to health care costs and care continuiity is ‘tagged documents’, the higly touted recommendation in the report to the President a few months ago.
See:http://www.whitehouse.gov/blog/2010/12/08/pcast-releases-health-it-report
And in the HITPC Stage 2 recs their is a requirement that at least 25 patients download their helath info for a provider to meet MU.
“EPs: patients are offered secure messaging online and at least 25 patients have sent secure messages online…Stage 3: Provide mechanism for patient-entered data (supply list);
Google may still get what they want…only thru the back door
GT.M will probably make more inroads when it supports windows until then you can host the front end on a local instance of windows but you have to have a server attached. Plus it would be nice for when I’m implementing WorldVista.
You’re dead wrong!
Consumers are no different than docs, they will use software that helps them get the job done. Docs don’t like EHRs because they claim it does not contribute to their business, but in fact takes business away via the productivity hit in this fee for service payment world. Consumers don’t use PHRs for they do not want a digitial filing cabinet for their records and frankly, the majority of the healthcare industry has been VERY RELUCTANT to let consumers have their records in a fully portable format.
One need only look to KP, the VA or Group Health Collaborative to see that consumers will happily, willingly and delight in the use of a PHR if it is something that is easy to use, provides value. But it also points to what is critical to the success of such, a direct connection to the physician, to the practice and likewise, the physician’s promotion of it’s use.
So maybe we need to tear down the artificial walls that exist and are promoted by comments such as yours ala “EHRs are good, PHRs are bad” and begin talking about one record, the Collaborative Health Record (CHR) wherein all stakeholders are participants and contributors. This is where we need to focus, this is where this industry needs to move towards if indeed we wish to begin to move to truly patient-centric care.
Regarding the Las Vegas conference schedule – HiMSS is not to blame for this one. It’s the tourist industry and hotel schedulers in Las Vegas. Hotels and convention centers do not want business shows over the weekends since Las Vegas is booked with party-goers and impromptu wedding seekers. Any conference in Las Vegas is week-day based due to the hotel schedule. This one is not the fault of HiMSS.
HIMSS staff will be staying over the weekend, as has always happened for every conference, including New Orleans.
Who do you think the biggest Party-Goers are?
DUH!
Peter,
Yes, you are certainly correct that HiMSS staff likes to party. However, one still must examine the numbers between HiMSS staff preparing for the show and conference attendees. This isn’t just a HiMSS issue; it’s a Vegas capacity and hotel revenue stream issue. And yes, it’s an inconvenience to not have the weekend days, but this is one where the blame cannot be laid solely on HiMSS.
I like John’s comments about a CHR. I believe this is the direction that should have been encouraged by all stakeholders right from the beginning.
The beginning, I mean as, that part of history when EHRS made the quantum leap from being just xerox copies and fax machines talking to one another and actually evolved to “Form Filler” technology. Which is basically where we are now, except its loaded up with vendor security features like digital watermarks, encrypted or vaulted user interfaces. We all know where this is leading. The big payoff by the king of bailouts… The Taxpayer is going to have to buy a universal user interface.
Re:”OptumInsight (formerly Ingenix) is awarded a patient for its LifeCode natural language processing technology”
Hopefully they get more than a “patient”
[From Mr. HIStalk] Your spell check is snarky, but slow. I fixed that typo Monday morning.