"Upon learning what I do, several attendees went into some pretty serious rants about how electronic health records have destroyed…
News 2/2/11
From Former CIO: “Re: PCAST report. It seems the PCAST report has been glossed over or dismissed as a bunch of government mumbo jumbo. The HIMSS response is once again laden with not-so-hidden vendor protection. This blog note hits the nail on the head.” Vince Kuraitis describes the organizational reaction to the PCAST report, which basically says we’re going in the wrong direction with today’s HIT systems. Those criticizing its conclusions include the usual turf-protectors: HIMSS, EHRA, AHA, FAH, RSNA/ACR, and IHE. I realized that I hadn’t provided highlights of the PCAST report, so scroll down for my summary and you’ll see why those groups don’t care much for the recommendations.
From AZ: “Re: MyChart. Tucson Medical Center has launched it for Saguaro Physicians along with Epic’s MyChart Mobile App.” Unverified.
From Dolphins Fan: “Re: Epic. There aren’t many spinoffs in the Madison area. Either they retain top talent, people leave Madison to start their businesses, or they have one hell of a non-compete.”
Speaking of unsurprising reaction to political events, eHealth Initiative releases a statement (I don’t have a link) urging that House Republicans keep the HITECH feed trough full instead of exercising fiscal responsibility. “We realize that the Spending Reduction Act represents a principled stand against government spending, but we would encourage Members of Congress to not use the HITECH Act or any of its provisions as a target, as that will only create further uncertainty in the health care sector. Any attempt to repeal funding for health information technology would have severely negative effects on public and private progress now and in coming years.”
Management changes at enterprise visibility vendor Intelligent InSites: president and CEO Mark Rheault resigns and the majority owner, an investment company, puts one of its people in the interim role until a successor is found. That guy is Doug Burgum, who took over Great Plains Software years ago and arranged its acquisition by Microsoft.
Thanks to Iatric Systems of Boxford, MA, joining HIStalk as a Gold Sponsor. The 20-year-old company has provided applications, interfaces and reporting solutions to over 900 hospitals (especially Meditech), has been recognized as one of the country’s fastest-growing companies, and has been named one of the top 100 businesses in the Boston area. Check out their YouTube channel, which features an interview with Denni McColm, CIO of Citizens Memorial Hospital (Stage 7 EMRAM, putting the tiny hospital in elite company), which used Iatric to integrate their Meditech systems with Google Health and a patient portal. They’ll be at HIMSS talking about interoperability, so plan to drop by, say hi, and thank them for supporting HIStalk. And of course for doing the cool HITECH Train parody video.
McKesson announces Q3 numbers: revenue flat, EPS $0.60 vs. $1.19. The company set aside $0.52 per share as a one-time expense for its continuing fight against drug Average Wholesale Price lawsuits that have already cost it a fortune. Without that charge, earnings would have been down but would have hit estimates and the company raised guidance for the fiscal year. Technology Solutions revenue was up 2%, but software revenue was down 2%. Still, that division made $106 million. It had $1.3 billion in unrecognized revenue, which could be great (lots of money coming) or terrible (it hasn’t been recognized because customer contract terms haven’t been met).
The McKesson conference transcript is here. John Hammergren says he doesn’t think ARRA money will be pulled out even if healthcare reform is successfully challenged, but that it doesn’t really matter at this point since customers are already committed.
HIMSS announces the recipients of its clinician IT leadership awards: Liz Johnson RN, VP of applied clinical informatics at Tenet (the announcement calls it “Tenant”) and Michael Zaroukian MD PhD, CMIO at Michigan State University.
A hospital in Australia doubles its eye tissue donations by monitoring the outbound ADT messages of hospitals to see if any designated donors have died, allowing tissue banks to be immediately notified. The application was built using InterSystems Ensemble.
We sometimes do interviews on HIStech Report when companies want to use the final product in handouts or downloads. I recently interviewed Mitchell Goldburgh from image management vendor InSite One, just acquired by Dell.
Weird News Andy fingers those Down Under: an upcoming journal article finds that Australian medical students are performing exams (genital, rectal, and breast) on unconscious hospitalized patients who have not been asked for consent.
Open source EMR vendor Tolven gets profiled in an article covering venture capital in California. British publisher Elsevier gave the company $3.6 million from its venture fund. The article says the company had $1 million in sales in 2010 and expects $2.5 million this year.
The regular company e-mail from Kaiser Permanente CEO George Halvorson has some interesting 2010 numbers: members logged in to its site 62 million times to get information, patients viewed 25 million lab tests online, doctors conducted 10 million secure message based e-visits, patients had 8 million electronic prescription refills, and 2 million visits were scheduled electronically. He concludes that people want online convenience instead of driving and telephone.
Wolters Kluwers Health is supporting HIStalk as a Platinum Sponsor, so thanks very much to them. The company has quite a lineup of clinician-familiar names: Facts & Comparisons and Medi-Span (drug references and databases); the ProVation ClinicNote custom content and documentation solution for EMR vendors; ProVation EHR for ambulatory surgery centers; ProVation MD for clinician procedure documentation; ProVation Multicaregiver perioperative documentation system with monitor interfaces; ProVation Order Sets, powered by UpToDate Decision Support for CPOE and paper order sets; and the fabulous UpToDate evidence-based clinical decision support system. Clinical content and order sets are important for improving outcomes and meeting Meaningful Use EMR requirements, so give them a look. Thanks to Wolters Kluwer Health for supporting HIStalk.
This happens all the time: a treatment assistant making $62,000 per year racks up $1 million in overtime pay over 12 years, making the state employee eligible for a pension (if you don’t work for government, you’ll probably have to look up the definition of that word) that will pay 50% more per year than he makes working.
PCAST Report Summary
This report was commissioned by the President and created by his Council of Advisors on Science and Technology (real scientists, not vendor people, HIMSS puppets, or the usual talking heads).
Healthcare IT’s potential:
- Integrate technology into practice without forcing doctors to perform data entry
- Provide clinicians with complete information at the time of decision making
- Get patients involved in their care
- Enable public health monitoring
- Speed up clinical trials
- Reduce administrative overhead
- Create jobs
- Support healthcare reform
But it isn’t working:
- 80% of physicians in practice still don’t us even a primitive EMR and interoperability is poor
- Need to take advantage of the network effect, which would require universal data exchange standards
- As a result, the market for new HIT-based products and services is underdeveloped
- Systems are proprietary, don’t work well with physician workflow, and weren’t built to exchange data in non-proprietary formats
- EHR users see their systems as purely internal – they have no incentive to open them up to patients, competing providers, or research organizations
- Privacy concerns are common
- Incentives are misaligned, so the only good reason to invest in HIT is if it improves administrative efficiency
Conclusions:
- Goals can’t be met with the modest interoperability requirements of HITCH and certification
- Putting more non-interoperable EMRs out there via HITECH will just make the problem worse
- Need a universal exchange language – tagged data elements (similar to XML – CDA is an example).
- Cost to develop the universal exchange language would be $20 to $40 million and the cost to vendors would either be a 5-10% increase in EHR cost or a one-time expense of $5-$20 million per vendor
- ONC and CMS need to step up the interoperability game for the 2013 and 2015 Meaningful Use requirements
- Services should be created to send and receive tagged data elements, which would eliminate the need to repose data in a national database
- The universal exchange language would open up markets for new tools and services, improve privacy, eliminate the need for a national patient identifier, and facilitate public health
- HIT is a mix of "the good, the bad, and the ugly"
Also:
- CMS itself has outdated systems and lack of internal knowledge about information exchange and replacement system proposals are just as inflexible (doctors have to submit data twice, for example, once to get paid and once for quality incentives)
- HIE progress is being slowed down by the complexity of developing their member agreements, the lack of financial incentive to improve outcomes, and their unclear capability to scale
- HIEs are "ill-suited as the basis for a national health information architecture" and only a handful have gone beyond the pilot stage once their initial grant money was spent
- Middleware that can extract information from proprietary EHR databases can help (dbMotion, ICA CareAlign, Medicity MediTrust, Microsoft Amalga, Oracle HTB, Orion Health)
- Examples of successful EHR adoption are VA and Kaiser, but even they can’t exchange information outside their organizations and since they are closed systems, they don’t create a market for innovation
- The problem with today’s EHRs: they don’t make the physician’s job easier and force doctors to type in their own information
- EHRs were built to look like electronic versions of paper forms without the involvement of usability experts, so they don’t provide much decision support
- Errors in diagnosis may be far more common than errors in treatment and EHRs don’t help much with that
- Quality measures are too specific and focus on medicine’s traditional emphasis on treating illness rather than coordinating care and maintaining health
- EHRs were built around billing codes, which don’t provide a patient-centered and historical view
Recommendations:
- Federal CTO Aneesh Chopra should within 12 months produce metrics to measure progress toward a national healthcare infrastructure, including pilots, and assess yearly
- ONC should require metadata-tagged data elements to meet 2013 MU requirements, publish standards for services that can access patient data, and work with the Small Business Administration to develop companies that could offer cloud-based services to small physician practices, LTFs, and hospitals
- CMS should move away from collecting data relating to lists of health measures and move toward higher levels of information exchange and clinical decision support
- AHRQ should be given funding to develop a test network for comparative effectiveness research and give medical researchers access to de-identified, near real-time data using data element access services
HERtalk by Inga
From Sales Professional: “Re: commissions. Every HIS vendor I’ve worked for (SMS, Data General, TSI, IMS, Eclipsys, HMS, McKesson, AGFA, and Keane) had commission plans that tied payments divided just as the license fees, i.e. you get your money when the client pays his bill. Albeit ‘golden handcuffs’ for the rep, this did link incentives for the rep to selling business that the company could install and get paid for. SMS, I believe, started this in the early ‘80s after a few reps got paid huge commissions and SMS could not deliver. After Sarbanes-Oxley, a lot of the bigger companies claim they need payment terms that the GAAP accounting rules can recognize, and most claim that a ‘holdback’ for post-live payments is NOT a bookable revenue item for them.”
DiagnosisOne appoints Kenneth W. Kizer, MD, MPH to its board of directors. He is former president and CEO of Medsphere Systems, the founding president and CEO of the National Quality Forum, and a former Under Secretary for Health for the VA.
Mediware Information Systems posts its Q2 numbers: net income of $1.73 million, compared to last year’s $783K; revenue of $13.2 million versus $10.8 million.
The board of directors of Harrison Medical Center (WA) approves a $7.6 million, 10,000 square foot data center to support the medical center’s new EMR (Allscripts Sunrise, I believe).
Venture capital investment for medical software and information services grew from $387.5 million in 2009 to $460 million in 2010. That’s a 19% increase.
NCH Healthcare System (FL) anticipates earning $11 million for its meaningful use of (Cerner’s) EHR.
Awarepoint says that 91 hospital sites contracted for Awarepoint’s RTLS products in 2010, a 30% increase over 2009. In addition, annual revenue growth exceeded 100%.
Newark Beth Israel Medical Center (NJ) licenses Meta Health Technology’s electronic clinical documentation improvement software.
The University of Texas MD Anderson Cancer Center purchases Carestream Health’s RIS system.
Streamline Health Solutions appoints Robert Watson as president and CEO, replacing founder and president/CEO J. Brian Patsy. Patsy retired at the request of the board and also resigned as a company director. Watson is the former president and CEO of DocuSys.
CareFusion names Kieran T. Gallahue chairman and CEO, replacing the retiring David L. Schlotterbeck. Gallahue was most recently president and CEO of ResMed.
Harold J. Apple takes over as CEO and president of the Indiana HIE. The HIE’s founding president and CEO J. Marc Overhage will remain on board as chief strategic office and national policy advisor. Apple is the former majority owner, CEO, and president of Vector Technologies.
Fifteen California hospitals adopt InQuickER, which facilities patient appointment scheduling for emergency rooms. Patients wanting to reserve a time in the ER typically pay a $15 to $25 premium for the service. At Lakewood Regional, the hospital pays $3,000 for the InQuick ER service and charges patients $15 to schedule an appointment. Lakewood’s ER sets aside only one appointment per hour and patients must reserve their spot at least two hours in advance.
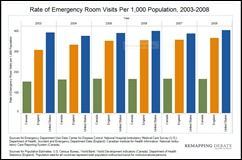
Speaking of ERs: between 2003 and 2008, the rate of ER visits in the US exceeded rates in both England and Canada.
OMG. It’s February and I am leaving for Orlando in 19 days. So much to do beforehand! I shared with Mr. H (who couldn’t even feign excitement) that I bought a new dress for HIStalkapalooza, but am still pondering over the shoe selection. Truth be told, I am afraid I’ll be “outed” if I were to were the fab shoes that would really make the ensemble. I am hoping that others attending will take their fashion selections as seriously as I am, especially since this year there are prizes involved. So ladies, find your best shoes and a sassy cocktail dress. And guys: women drool over men in tuxes, especially when the IngaTinis are flowing. And, keep in mind that it’s hard to look hot when you are wearing a shirt that screams your company’s name. Just sayin’.
Versus Technology introduces Enterprise View Mobile for use on the iPhone, iPod Touch, and iPad. The free application gives users access to patient, staff, and equipment locations on mobile devices.
Former Cerner COO Paul Black joins the board of Netsmart Technologies.
Poudre Valley Health System CIO Russ Branzell tells the local press that PVHS will spend between $30 and $40 million on its EHR investment (Meditech). He also admits that their EHR stimulus reimbursement will be “nowhere close to the investment we put in.”
Sponsor Updates by DigitalBeanCounter
- Denver Health engages MEDSEEK to develop and deploy its new patient portal.
- T-Systems and Medicity separately announce the successful validation of their interoperability expertise at the recent North America Connectathon.
- DIVURGENT managing partner Colin Konschak co-authored the recently published book, Accountable Care Organizations: A Roadmap for Success. Guidance on First Steps.
- CynergisTek announces that its revenues grew 33% in 2010, which included a 10% jump in existing client revenues. New client revenues accounted for 48% of 2010 revenue growth and technology partner solutions revenues grew 265% over 2009 performance, accounting for 50% of total revenues.
- Janet Dillione, EVP & General Manager of Nuance Communication’s Health Care Divison, is featured in this week’s Forbes technology section.
- Several EHR vendors, including NextGen and eClinicalWorks, are mentioned in an Information Week healthcare article titled How 7 Vendors of EHR Systems Measure Up.
- Design Clinicals announces its contract with St. Patrick Hospital and Health Sciences Center (MT), where it will implement MedsTracker for medication reconciliation.
- Florida Hospital Celebration Health chooses the interactive patient care solution of GetWellNetwork.
- API Healthcare announces the release of API Healthcare Syngergy, a workforce management solution.
- Forest Park Medical Center (TX) chooses Access Intelligent Forms Suite to replace pre-printed forms with on-demand e-forms that include printed and barcoded Meditech data.
- St. Joseph Medical Center (MD) selects Provation MD for gastroenterology procedure documentation and coding.
- Florida Academy of Family Physicians recommends Ingenix CareTracker to its members.
- MEDSEEK will develop and deploy Denver health’s new patient portal.
EPtalk by Dr. Jayne
What a difference a year makes! This week, I spent time with a family member in a hospital across town, which incidentally has a large integrated clinical system different from my own. I was last there with another family member about a year ago, not long after the hospital went live.
At that point, the staff was still fairly hostile and frustrated, having just come off of weeks of training and feeling very stressed. Knowing that I work for a competitor hospital, and knowing what I do, many of them went out of their way last year to tell me how much they hated the system. This week was the completely opposite side of the pendulum. No one was saying anything about the system. I was puzzled: could it really be that good? Or had they just all been assimilated?
Being the investigator I am (probably watched too many episodes of “Quincy, M.E.” as a kid) I “accidentally” left my name badge from Enemy Hospital on my collar the next day, to see if anyone took the bait. Nothing. Finally, I asked the nursing staff what they thought. Had they reached Nirvana? Had all the issues been fixed?
The answers I received were what could only be described as a completely mixed bag. Although some of them feel that the system has changed for the better, others still perceive it to be largely the same as it was a year ago, but they’ve learned to use it as a patient care tool like any other. One self-aware nurse commented that she didn’t really hate the system at first, it was just the idea of it, and it wasn’t worth the energy to keep complaining about it.
That’s the central challenge of most of us that are in the implementation and support business have to figure out – how to determine which users are going to be like that nurse gradually accepting the system vs. which users are going to rage against it regardless. This is the magic of figuring out which of the 20% of users will ultimately need 80% of your attention, and finding a way to help them adjust.
One thing I found interesting about the experience was that only the health system-owned primary care practices are on the system, and they have no health information exchange with their community and subspecialty docs. The specialty physician caring for my relative walked in with a (gasp!) paper chart from his office, after walking it out the door and across the campus, sans audit trail, sans security, and with wild abandon.
After I recovered from the delirious thought that it would probably spend the night in the trunk of his car, mingling with other deviant charts, I asked him why he was still on paper and whether they planned to switch any time soon. It turns out they are, having finally succumbed to being purchased by the health system after a protracted battle with one of their major insurers.
It will be interesting to see how much difference the next year makes for them. They are not only losing their autonomy to a major health system (and boy, do I wish my system had snapped them up instead — his group is incredibly fun at parties) but also giving up their paper. Theirs is just one of thousands of practices that will go through one or both of those transitions in the next several years as Meaningful Use unfolds. I’m sure I’ll be offering them a shoulder to cry on at some point.
Speaking of crying, those were tears of joy as I responded to a deluge of Facebook friend requests last week. I was starting to have a bit of the winter hum-drums, but my new BFFs seem to be extremely entertaining. I also heard from the team at NextGen, vendor of the system used by my not-so-secret crush, Dr. Robert Murry. They’ve offered to put us in touch. Do I sense an interview in my future?
I’ve received several great “Dear Dr. Jayne” questions this week, but I am holding out for something sassy, so feel free to send those deep, dark questions my way!

Have a question about medical informatics, electronic medical records, or whether nurses ever yell at doctors? E-mail Dr. Jayne.













Mr HISTalk – on PCAST – you are partly right, but partly wrong on who is behind PCAST. It didn’t have the “typical vendor” or “puppets” – it had the grand master puppeteer – Craig Mundie from Microsoft with several Microsoft or Microsoft funded panels.
Also, check out which of the “real science” people on the leadership team receive funding from Microsoft or the Bill and Melinda Gates Foundation.
This report is a highly orchestrated sales pitch for Amalga and HealthVault.
PCAST meetings are generally supposed to be public meetings – ask for the transcripts for all the meetings behind this report and read them.
Also, a fun puzzle, find out who put fingers to keyboards and actually wrote the report. Insiders say it was authored by Microsoft staff when they couldn’t make progress on a recommendation.
It is a reasonable statement of some of the challenges of healthcare, but if those who are suggested in this report as possible saviors are so well positioned to save us, then why have they waited so long?
20 to 40 Million for a Universal Exchange Language? Charge the current vendors 2 to 5 Million? We’re going over the socialist cliff on this one. And, why doesn’t ONC support an existing standard like SnoMed and HL7 RIM/CDA – we say it’s too complex and want to support CCR instead and yet here we say we need comprehensive coverage and definition of a healthcare data model?
This is one worth digging into? Anyone who knows how to navigate the government FOIA process should dig to figure out who is behind this report and where their self interest lies. You’ll likely not have to dig deep.
PCAST Report: From the link above to Vince Kuratis’ blog, I don’t see how the positions of IHE and CGC are any different, yet IHE is depicted as espousing a “bury PCAST” position, while CGC’s position is supposedly “PCAST has some great ideas”.
For some informed critique on the PCAST report, I recommend Keith Boone’s blog, http://motorcycleguy.blogspot.com/2010/12/my-review-of-pcast-report-on-healthit.html and http://motorcycleguy.blogspot.com/2010/12/language-of-healthit.html , as well as David Clunie’s analysis of the mammography use cases from the report: http://dclunie.blogspot.com/2010/12/imaging-and-pcast-presidents-council-of.html
“Need a universal exchange language – tagged data elements (similar to XML – CDA is an example). ”
Having built a number of CDA interfaces I can tell you there is nothing standard about it. It’s still a model, and developers get to model their data the way they see fit. There is a reason there is an A in CDA. Architecture, it’s far from being useful as a universal exchange language for healthcare. It has it’s place in moving medical documents. It’s too complex for general use. Using tagged elements is no better than using HL7 v2 messages.
“Middleware that can extract information from proprietary EHR databases can help (dbMotion, ICA CareAlign, Medicity MediTrust, Microsoft Amalga, Oracle HTB, Orion Health)”
If you want the cost of interfacing to go even higher, and have even more problems take this approach. Hacking into another vendors database is not a solution, it’s a hack. If you want the cost of interfacing to go down and be more reliable, vendors need to lower their interface costs to a reasonable amount. Asking $6k-$40K for a feed of ADT data out of your system seems a little high.
I saw a quote last week for a Meditech interface to create CCD. $100k. The first time you try to feed that CCD to a referring physician, guess what, it’s not going to import all of the data correctly into their EMR. So you’ll ask Meditech to make a change, and for $10k-$40k maybe they will. Or you’ll run it through an engine just like your HL7 v2 messages to make the interface work.
I agree HIT can be improved, and some of the suggestions above are good ones, but some are way of base, and clearly come from people living in an ivory tower, and not the real world of data exchange.
Re: your commentary on eHealth Initiative statement on proposal to cut HITECH funds. You couldn’t be more wrong — whether you like the HITECH program or not, or you like eHI or not, pulling the rug out from under the provider community now would be disastrous. I say that as someone who won’t be directly affected one or the other if the HITECH funds are cut…..
ILiveInTheRealWorld – hit the nail on the head. CDA is no more than XML wrapped up in HL7.
Also point to point interfaces in general create not remove problems with healthcare infrastructure. It’s just another silo of data to maintain and support. HL7 interfaces should be kept to a minimum. It’s not the cost of the interface, but the cost of the staff to check for errors and maintain disparate coding structures.
A fundamental change of architecture and infrastructure is required and is possible with most EMR vendors. This whole “closed system” hasn’t been true of the big three for some time now most having the ability to implement SOA. SaaS and Cloud? Meh. SOA has far more bang for the buck in larger organizations.
If you believe PCAST isnt driven or influenced by “vendors” who lurk underneath the covers…then you probably believe Obamacare is about improving quality and access to care.
There is no healthcare initiative, neither technical, operational, or financial, that is born and driven absent of a corporate beneficiary, including the Fed.
Congrats to Histalk- finalist in medgadget’s Blog awards, in the category of best medical technologies/informatics blog:
http://www.medgadget.com/archives/2011/01/the_2010_medical_weblog_awards_finalists_sponsored_by_epocrates_and_lenovo.html
voting starts tomorrow!
For those HISTalk readers interested in AMIA’s response to the PCAST report, pdf found here: https://www.amia.org/files/AMIA-PCASTComments-Submitted-to-ONC-1-19-11.pdf. Cheers!
Why do continually post HIMSS news no one but HIMSS cares about:
“HIMSS announces the recipients of its clinician IT leadership awards: Liz Johnson RN, VP of applied clinical informatics at Tenet”
Everyone in this field, including you, know Liz Johnson is not only on HIMSS BOD for years, but also on David Blumenthdl’s HHS Standards Committee and HHS Policy Committee, as well as having input on the HHS Privacy & Security committee.
Why do you withhold the obvious?
I am beginning to question your own affiliation with HIMSS. Does HIMSS pay you advertising $$$ to mention them??
[From Mr. HIStalk] I’ll let the wisdom of your comment speak for itself.
re: McKesson revenue stream
$1.3 billion is an impressive number. to answer Mr. H’s question, it’s from unrealized revenue. like most large vendors, McKesson doesn’t realize income until products are actually implemented. as was mentioned by someone on here a few days ago in regards to sales commissions, when a hospital closes a $10 million deal, the vendor doesn’t see any of that on the day of the close. it’s incrementally realized over time. it’s a good model for both the company and the hospital, who doesn’t get swindled if the company never implements the product or even goes bankrupt before they implement it. personally, I think every vendor should have the same policy, but I know there are some that expect payment to be front-loaded shortly after contracting. my reading of that transcript is that McKesson is actually in great financial position both overall and within their technology division. no wonder the stock price shot up yesterday after the report came out!
I read only portions of the PCAST and still kind of mystified at how the estimate of $20-$40M for a ‘universal language’ was derived. Don’t dispute it as much as I am still kind of foggy on how they get their and costs associated with specific tasks.
As for the interfaces, they are an inevitable reality in any large organization with a host of different types of IT applications and legacy solutions. The killer though is that the cost of creating interfaces in the healthcare industry is generally lucridious (e.g., $5-$7K for even the most basic lab interface into an ambulatory EMR vendor) and the maintenance costs in terms of staff/consultant/vendor fees associated with the constant maintenance, testing, and other issues associated with them. It is a festering sore on your IT budget that never really goes away once you create it.
Agree with blah. SOA is generally the answer but the problem is that most HIT vendors are just gradually moving to that or still haven’t adopted it. Doesn’t do much good though for the hospitals, physician offices, and providers though that have purchased older solutions.
From Dolphins Fan: “Re: Epic. There aren’t many spinoffs in the Madison area. Either they retain top talent, people leave Madison to start their businesses, or they have one hell of a non-compete.”
Ding, ding, ding – correct answer is number 3, they have a helluva non-compete.
It is pathetic that the direction of this country in HIT was guided by the trade group for the industry, HIMSS and its prior subsidiary, CCHIT. It seems that the path taken has raised concern as noted in PCAST (that premise is a good one, even if conflicted), and by the HR 408 to defund HITECH and Meaningful Use.
The NY Times wellness blog features a nurse who is now caring for computers rather than patients. Can not the vendors make these devices usable any more?? That is “big f’n deal” as our VP has been heard to say.
Re: PCAST summart – EHRs were built to look like electronic versions of paper forms without the involvement of usability experts
I think it’s the reverse. EHR’s were built to look like inventory systems and thus cause cognitive overload.
Show me paper forms that look like these.
If paper forms were emulated, the usability and usefulness might actually be better than what we have now…which is thoughtless design.
— SS
Re: TPD speculation on why Blumenthal is leaving. Why do you dignify such drivel? This was all known from the start. Harvard gives tenured professors 2 years away from campus before they lose their chairs. It’s why Larry Summers went back when he did. It’s why David Blumenthal is going back now.