HIStalk’s Guide to ViVE 2024
Care.ai
Booth 1402
Contact: Lexi Lutz, marketing manager
lexi.lutz@care.ai
407.800.1937
Care.ai is revolutionizing healthcare with the world’s first and most advanced AI-powered Smart Care Facility Platform and healthcare’s leading Always-Aware Ambient Intelligent Sensors. Care.ai transforms physical environments into self-aware smart care spaces, increasing safety, efficiency, and quality of care in acute and post-acute settings while at the same time autonomously improving clinical and operational workflows and enabling new virtual models of care for Smart Care Teams, including Smart-From-The-Start Virtual Nursing solutions.
CereCore
Contact: Jillian Whitefield, business development manager
Jillian.Whitefield@CereCore.net
248.891.5557
CereCore is a proud sponsor of Club CHIME, so drop by the Club CHIME Lounge for some refreshment, swag, and to connect with our experts. Schedule a meeting with us on Feb 26 or Feb 27 from 8 a.m. – 6 p.m.
CereCore works behind the scenes to empower hospitals and health systems with IT services around the nation and globe. Looking for IT and application support, technical professional and managed services, strategic IT consulting and advisory services, or EHR consulting? We should meet if you are interested in EHR experts, technical and support teams to supplement yours, looking for the right talent so you can better manage IT operations, or searching for support desk solutions that will result in happier users and providers. Find meaningful change with CereCore’s healthcare IT managed services. Let’s connect at ViVE 2024.
Clearsense
Booth 1702
Contact: Larry Kaiser, chief marketing officer
lkaiser@clearsense.com
516.978.5487
Get ready to rock at ViVE 2024! This exclusive event is where digital health execs connect with our 1Clearsense healthcare data analytics and interoperability platform. At ViVE, you will find us at booth #1702, in the Hosted Buyer Meeting program, and rocking Industry Night as a proud co-sponsor of an exclusive concert with legendary punk rocker Billy Idol.
Clearwater
Booth 1549 in the Cybersecurity Pavilion
Contact: Julie Catron, director, product and content marketing
julie.catron@clearwatersecurity.com
217.620.0874
Healthcare’s largest pure-play cybersecurity and compliance firm, the Clearwater team is excited to meet you at ViVE 2024! Regardless of where you are in the healthcare ecosystem, we’re committed to helping you move to a more secure, compliant, and resilient state. Whether you’re looking for ideas, help with a stand-alone initiative, 24/7 SOC services and incident response, or someone to partner with you through a true managed services program, we’d love to talk with you.
As a title sponsor of the Cybersecurity Pavilion, share some exciting things we’ve been working on. Here are a few of the things you won’t want to miss at our booth:
- Monday, 2/26, 10:40 in the Cyber Pavilion – Chasing a Cyber Attacker: A play-by-play recount of threat detection and response and lessons learns about improving cyber resiliency.
- Monday, 2/26: 1:30-2, Tuesday, 2/27: 10-10:30 2-2:30 – How Academy Medtech Ventures Navigates Cybersecurity, Compliance, and Sustainable Growth in Digital Health: Come meet AMV President JJ Mosolf as he demonstrates their cutting-edge Operating System of Cognition and shares how cybersecurity has been critical to scaling this digital health company quickly.
- Information and giveaways at booth 1549.
Clinical Architecture
Booth V2537
Contact: Jaime Lira, VP of marketing
jaime_lira@clinicalarchitecture.com
317.580.8400
Please join us on Tuesday, February 27 at 10:45 a.m. PST for a 30-minute case study presentation “Where Data Quality and Master Data Meet” featuring Will Lloyd, System Director Clinical Data Governance at CommonSpirit Health and Charlie Harp, CEO at Clinical Architecture in the InteropNOW! pavilion.
Clinical Architecture delivers data quality solutions for healthcare enterprises focused on managing vast amounts of disparate data to succeed with analytics, population health, and value-based care. Our industry-leading software provides semantic interoperability of data through robust content authoring, mapping and distribution architecture at speed and scale.
DrFirst
Booth 1830
Contact: Erin Lease Hall, senior manager of events
eleasehall@drfirst.com
216.650.7687
Visit DrFirst at ViVE! Where Digital Health Execs Go to Redefine Medication Management What if less work – with up to 80% fewer clicks and keystrokes – is the key to getting your clinicians the clean, complete medication data they need? If that sounds implausible, it may be time to redefine medication management. And we can help. Heading to ViVE 2024 in Los Angeles? Stop by booth 1830 and learn how redefining medication management with better patient data can boost patient safety and outcomes to transform your business. Not heading to ViVE? Not to worry. We can still talk redefining medication management. Schedule a meeting with us.
ELLKAY
Booth 1336
Contact: Auna Emery, VP of marketing
Auna.Emery@ELLKAY.com
201.808.9504
ELLKAY’s innovative, cloud-based solutions address the challenges that our partners across all healthcare environments face. ELLKAY delivers bi-directional, standards-based connectivity to hundreds of sources with access to discrete and actionable data, and provides tailored solutions to achieve your unique connectivity goals. Don’t miss our InteropNow! sessions with CommonWell Health Alliance at the InteropNow! Pavillion:
- “Behind the Curtain of the 226M+ Persons National Network – CommonWell Health Alliance – powered by ELLKAY.” Get a glimpse of the interworking’s of CommonWell’s national network powered by ELLKAY, serving over 34,000 provider organizations to enable seamless health data exchange across member organizations, nearing close to 226 million+ individuals impacted through this network. The CommonWell Health Alliance chose ELLKAY to serve as the Technical Service Provider to enable clinical data exchange at scale and serve as a critical partner to achieve QHIN designation under TEFCA.
- “CommonWell Health Alliance- powered by ELLKAY.” Understand how CommonWell Health Alliance is using ELLKAY to fuel the connectivity for its network. Get to know more about the updates to the CommonWell platform and how ELLKAY is providing the technical infrastructure to deliver a seamless patient data exchange to participating providers. Come learn who the CommonWell Health Alliance members are and the impact of participation in this national network.
Visit Team ELLKAY at booth #1336 – Mimosa Bar, Monday, February 26, 3:30-6:00 p.m., Ice Cream Bar, Tuesday, February 27, 3:30-6:00 p.m., Donut Bar, Wednesday, February 28, 8:30-10:30 a.m.
Five9
Booth V946
Contact: Roni Jamesmeyer, senior healthcare marketing director
roni.jamesmeyer@five9.com
972.768.6554
Five9 offers a HIPAA-compliant healthcare cloud contact center solution that empowers you to seamlessly monitor and report call volumes in real-time across critical areas such as patient access, scheduling, prescription refills, and revenue cycle management, enhancing your staff’s efficiency. The Five9 Intelligent Cloud Contact Center seamlessly integrates with various back-end systems, including electronic health records, serving as a central hub to facilitate digital engagement, provide comprehensive analytics, optimize workforce performance, and leverage AI for improved outcomes and measurable business success.
Fortified Health Security
Booth 1850
Contact:Robert Pullins, growth marketing manager
rpullins@fortifiedhealthsecurity.com
615.600.4002
A two-time Best in KLAS award winner, Fortified works with healthcare organizations to construct client-centric, customized programs leveraging both new and existing solutions. We are committed to building a stronger cybersecurity landscape for both our client ecosystem and the healthcare industry as a whole.
We are Healthcare’s Cybersecurity Partner and we’re coming to ViVE with a schedule full of collaboration and socializing! We hope you can join us for one of these events:
- 3-track Tasting at the Figueroa: From 5-8 p.m. on Monday, February 26, CISOs and CIOs are invited to join us in hotel Figueroa and select a tasting track of spirits, wines or mocktails led by Blackfin Experiences sommelier Michael Stefanakos. Contact us to RSVP at connect@fortifiedhealthsecurity.com.
- CHIME members only: Focus group titled “Future-proofing healthcare IT: A collaborative discussion on HHS’s new cybersecurity strategy” held Sunday, February 25 at 10 a.m.
- Daily drawings at booth #1850 for travel JBL speakers.
Get-to-Market Health
Contact: Steve Shihadeh, CEO
Steve@gettomarkethealth.net
610.613.4074
Get-to-Market Health is a specialized consultancy focused exclusively on accelerating sales and driving revenue growth for our healthcare technology clients. We work with business leaders to simplify the complexity and unique buying patterns of the healthcare technology market.
Healthcare IT Leaders
Booth 3123
Contact: George Major, RVP of sales
george.major@healthcareitleaders.com
484.682.3614
Healthcare IT Leaders is a national leader in IT staffing, managed services, and consulting for healthcare systems. We provide strategy and talent for healthcare transformation across clinical, business, and operational systems. Areas of focus include EHR, ERP, HCM, WFM, RCM, Cloud, and Data where our consultants implement and optimize enterprise software solutions from leading vendors including Epic, Oracle Health, Workday, UKG, Oracle, Infor, SAP, Snowflake, AWS, Azure, GCP, and more.
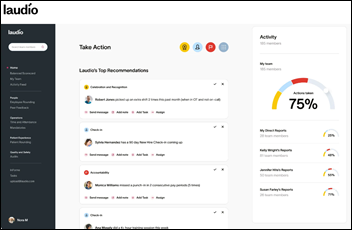
Laudio
Meeting Pod 2852
Connect with Laudio on-site. Tuesday, 2/27 at 10am: Join UNC Health CHRO Scott Doak, and Laudio co-founder and CEO Russ Richmond, MD, as they share their Playbook for Nurse Retention. Discover how UNC Health’s approach with Laudio’s automation software improved nursing management and reduced nurse turnover, leading to $5.4 million in annual savings.
Laudio empowers healthcare leaders to drive large-scale change through everyday human actions. Our AI-enhanced platform streamlines workflows for frontline leaders, strengthens interpersonal connections, and aligns C-suite objectives with frontline efforts, boosting operational efficiency, employee engagement, and patient experience. Laudio makes it possible for patients, frontline workers, and health system leaders to thrive together. Discover how at www.laudio.com.
Linus Health
Contact: Laura Kusek, event and partner marketing manager
events@linus.health
954.825.8389
Chief Growth Officer Curt Thornton and Chief Product Officer John Showalter, MD will be in attendance. Please email events@linus.health to request a meeting.
Linus Health is a digital health company focused on early detection of Alzheimer’s and other dementias. We combine rich clinical expertise with cutting-edge neuroscience and AI to help providers spot and intervene on early signs of cognitive impairment – even those invisible to the human eye. Our digital cognitive assessment platform puts specialist-level insights about a patient’s cognitive function at providers’ fingertips in a matter of minutes.
Medicomp Systems
Booth V1337
Contact: James Aita, director of business development and strategy
jaita@medicomp.com
647.207.0080
Clinical AI has healthcare abuzz. But how can you harness it to help make clinicians’ lives easier? Large language models (LLMs) are great at generating text, but clinicians need solutions to help them navigate compliance and quality reporting and complex billing requirements. The Quippe Clinical Intelligence Engine leverages LLM output, converts it into actionable data, and makes sense of it to help clinicians find what they need at the point of care to make their jobs easier. Meet with at Vive booth V-1337 to learn more about Medicomp’s clinical-grade AI solutions and Smart-on-FHIR apps for CQM compliance, HCC coding and risk adjustment, bi-directional interoperability, CDI and audit-readiness, point-of-care decision-making and more.
MEDITECH
Booth 1524
Contact: Rachel Wilkes, director of marketing
rwilkes@meditech.com
781.774.4555
From the deployment of the latest AI solutions to industry-leading efforts in precision medicine and interoperability, discover how MEDITECH is making its vision for healthcare transformation a reality at ViVE 2024. MEDITECH staff and executives will be available at booth #1524 to discuss new Expanse tools for addressing key industry issues including: mobility, precision medicine, innovative care models, efficiency of care teams, interoperability, and AI.
In addition to activities in the booth, MEDITECH executives will also be speaking as part of the ViVE agenda:
On Monday, February 26 at 3 p.m., LACC, Show Floor, Venice Beach Stage MEDITECH’s Executive Vice President and Chief Operating Officer Helen Waters will be joined by leaders from Oracle and Epic for the “Back to the Future of Healthcare: Tomorrow’s EHR Landscape” session. They will discuss the future of healthcare and the transformative impact technological advancements have on patient experience and healthcare delivery.
MEDITECH Senior Director of Interoperability Market and Product Strategy Mike Cordeiro will host a session on Intelligent Interoperability on Monday, February 26 at 2:15 p.m. at the Tech Talk Stage. His presentation will focus on how EHRs should operate as data platforms – collecting, integrating, managing, analyzing, and presenting data in meaningful and actionable ways. Cordeiro will also highlight MEDITECH’s strategy for supporting interoperability standards and open API approaches that enable healthcare organizations to share meaningful data.
MEDITECH customer leaders will also participate as panelists in ViVE sessions, including: On Monday, February 26 at 2:00 p.m., LACC, Show Floor, Sunset Strip Stage Emanate Health Chief Information Officer Daniel J. Nash, MBA, PMP, CHCIO, CDH-E will discuss healthcare’s post-pandemic financial and workforce challenges in the session “Inside Job: Operating with Lean Staff and Healthy Margins.” The healthcare leaders will share cost-control strategies including workforce optimization and utilization of technology to enhance operational efficiency. HCA Healthcare Senior Vice President and Chief Information Officer Marty Paslick will join other panelists in discussing the ethical considerations, possible biases, and other challenges with AI in medical decision-making in the session “Awakenings: The Perils of AI Success” on Monday, February 26 at 4 p.m., LACC, Show Floor, Hollywood Stage. Attendees will learn more about the importance of responsible implementation to ensure patient safety and privacy.
QGenda
Booth 2112
Contact: Dan Kamyck, senior director of growth marketing
Dan.Kamyck@qgenda.com
770.399.9945
As a CHIME Foundation Member, QGenda executives will also be available for meetings at Club CHIME, located at Booth 2801.
Healthcare workforce optimization starts with the schedule. QGenda transforms healthcare workforce management with QGenda ProviderCloud, a single platform to activate, deploy, and optimize the entire care team. QGenda executives are on hand to help you manage change within your healthcare workforce. CHIME members – Be sure to sign up for QGenda’s Focus Group session, “Navigating Change: Digital Transformation to Optimize Your Workforce,” which will take place on Sunday, February 25 at 1:15 p.m. PST. To attend, please sign up with CHIME.
ReMedi Health Solutions
Contact: GP Hyare, managing director
g.hyare@remedihs.com
281.413.8947
ReMedi Health Solutions is a nationally recognized, physician-led healthcare IT consulting firm specializing in peer-to-peer, physician-centric EHR implementation and training. We’re a clinically driven company committed to improving the future of healthcare. We’re passionate “Clinician Whisperers” that believe understanding the “why” behind each EHR decision is as important as the “what” or “how”. We listen to physicians, nurses, and healthcare leaders in order to understand their biggest challenges, and we leverage our decades of experience to develop efficient solutions that greatly impact the delivery of care.
ReMedi designs customized training solutions that incorporate clinical workflows, evidence-based content, financial performance, and patient experience. Our clinicians and management consultants work with clients to: Improve physician satisfaction and engagement by enhancement of workflow and enabling efficient use of available tools. Enable physicians to more easily and accurately document patient conditions, comorbidities and acuity. Improve financial performance by capturing patient complexity. Evaluate reporting capabilities which allow the tracking of provider documentation and implications for the revenue cycle. Improve intra- and interdepartmental workflows between registration, physicians, and coding.
Rhapsody
Booth 2423
Contact: Michelle Blackmer, marketing
Michelle.Blackmer@Rhapsody.Health
312.520.1873
Visit Rhapsody at ViVE! Heading to ViVE 2024 in Los Angeles? Stop by booth 2423 and learn how health systems and digital health teams rely on Rhapsody to reduce the barriers to digital health innovation adoption by streamlining patient data access. Not heading to ViVE? Not to worry. We can still talk digital health enablement. Schedule a meeting with us.
Tegria
Booth 1624
Contact: Kristin O’Neill, senior director of external relations
kristin.oneill@tegria.com
617.319.5516
Tegria is a global healthcare consulting and services company delivering end-to-end solutions that leverage technology to help provider and payer organizations transform healthcare. Let’s schedule time to connect at Tegria’s Transformation Hub, located at booth 1624! Tegria solution experts will be available throughout the event, so this would be a great opportunity for us to brainstorm about solutions to your latest challenges. Schedule time to connect with us.
- Tech Talk: “Scoring Big on Patient and Provider Experiences.” Monday, February 26 at 2:30 p.m. PT Mark your calendar and join Tegria at the Tech Talk Stage as we discuss the importance of taking a team-based approach to patient experience. Join us for this must-attend session to explore how a collaborative approach can transform healthcare delivery.
- Happy Hour at the Tegria Transformation Hub Monday, February 26 at 4 p.m. PT After a full day of sessions and networking, stop by our Transformation Hub at booth 1624 beginning at 4:00 p.m. where you’ll be able to swap stories from the show floor, share your thoughts about a particularly interesting session you attended, or just unwind with some of your favorite Tegria experts.
TrustCommerce, a Sphere Company
Booth 1249
Contact: Ryne Natzke, chief revenue officer
rynen@spherecommerce.com
Visit TrustCommerce at Booth #1249! TrustCommerce provides comprehensive patient card payment solutions integrated with top EHRs that has earned the trust of many of the largest healthcare organizations in the US. Transform the way you process payments with TrustCommerce’s 20+ years of expertise in healthcare provider support. Experience secure and compliant payment processing, anytime and anywhere – all while being seamlessly connected to leading EHRs like Epic, Veradigm, and AthenaIDX. Meet our team, enter to win an Amazon Echo Show, catch a demo, and pick up some cool swag at booth #1249. See you there!
Upfront Healthcare
Booth 2130
Contact: Margy Enright, VP brand strategy and experience
menright@upfronthealthcare.com
913.568.1520
Upfront is a mission-driven healthcare company delivering tangible outcomes to leading healthcare systems and provider groups. Its patient engagement platform makes each patient feel seen, guiding their care experience through personalized outreach. The backbone of the Upfront experience is its data engine, which analyzes clinical, sociodemographic, and patient-reported data. These insights, along with its advanced psychographic segmentation model, allow Upfront to individually activate patients to get the care they need while building a meaningful relationship between the patient and their health system. Upfront is rooted in partnership, leveraging best-in-class healthcare expertise to maximize the impact of technology and deliver a next-generation patient experience.





































































Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…