HIMSS24 Comments
Responses were evenly split between vendor and non-vendor attendees. The average rating of HIMSS24 was 3.4 on a five-star scale.
What did you like best?
- Felt less crowded in a good way. Some education sessions were solid. Good networking with peers from other health systems.
- I didn’t see many double decker booths, which is perhaps a reflection of current fiscal climate.
- HIMSS tried to copy the Hosted Buyer format, but in a very limited way.
- Opening reception was too loud and there was no awards reception / banquet this year.
- Seeing and talking with current customers. That’s hands down the best part of HIMSS. The next best part was the puppy area.
- Always look for the first time exhibitors and visit their booths, to learn about their product offerings, and discern their rationale for paying the exorbitant fee for tiny space, travel, and lodging. Did they feel it provided ROI?
- Volunteered (did not take the gratuity) for focus groups to listen to vendor thoughts and attempts to discern the future. And to hopefully help them to understand my world, and that of my patients.
- The pre-conference workshops were well done and the new best part of my week.
- There seemed to be fewer attendees, which from an attendee standpoint, was good for me. Hotel rooms were more accessible — I heard people were able to book rooms only a few weeks before the conference.
- Better educational sessions.
- Loved the entrance to the floor with the tunnel and many photo ops. Need a photo booth where people or groups could take their photo and post on Instagram etc. The floor was beautiful, unlike Chicago, which had uncarpeted floors in the walkway, which was painful on feet and dirty feeling. It would be nice if there were a HIMSS person taking group photos or a standalone photo. Social media has improved. I liked how people had templates on their LinkedIn that they were going, but I never received instructions on how to do this.
- Better exhibit hall energy than last few conferences.
- The mobile app was helpful in sending reminders for appointments and announcements. Wayfinding also very helpful on the app.
- I really enjoyed the variety of speakers that were on the agenda. I also felt that the venue was better than Chicago, as there were more food options at the convention center, although the prices were outrageous. I also liked the private meeting areas that were available. It’s difficult to hold a meeting when there is so much noise and conversations taking place.
- Having carpet was a big improvement.
- Facilities and amenities. They’re feeling competitive pressure from HLTH and ViVE and it shows in their ice cream socials, puppy parks, and “fun” events.
- I like that the event has shrunken a little – it’s less overwhelming than it was in past years. Lots of food options in the exhibit hall, although expensive.
- I liked that there was a main stage on the exhibit floor like ViVE so people with booth meetings can go between them and educational sessions more readily. It’s also nice to see more clinical /burnout or hot issues addressed rounding out all the AI, cyber, and cloud topics.
- Great energy in the exhibit hall. Traffic was consistent right until Thursday afternoon, which is a first in my experience.
- It seemed smaller, so there were chairs available in sessions. Some years, rooms were so packed there were no seats. It was possible to get through the crowd without literally knocking into people.
- There seemed to maybe be more tracks this year, so the variety of sessions was good.
- Orlando is a better location as well than Chicago as you can walk more easily to and from hotels in Orlando.
- I was particularly impressed by the educational opportunities this year. A bit more practical.
- The app.
- Lobby looked good. Everything else seemed like it went backwards.
- Oddly enough, the government run talks were the most entertaining to me. Well thought out and with a bit of humor.
- Haha – there was edge to edge carpet throughout the exhibit hall, unlike last HIMSS. Seriously, there was good energy in the halls, attendance and interest was up over prior years.
- Still a boat/car show, but a little more manageable this year.
- My first HIMSS since 2019. The networks and meeting opportunities still valuable. Loved the booths that had AI displays.
What would you like to see changed?
- I would love to see floor hours shortened. The last hour is painfully slow while most people are either gathered around the booths with booze, or have already left.
- Coffee, water stations, and a food court, for the love of!
- Organize the floor or use some methodology for grouping solutions together. It is total chaos. People could evaluate and see more solutions quicker and might even learn about someone new. So many small companies (ours is very large) that do not even get seen.
- The Junior Wolf pack. Avoid Hal and his pontificating pals of their accomplishments.
- Have people who know what he hell they are talking about manning the booths. This was the exception vs the rule but I ran into so many CMF’s (clueless mf’ers) standing around playing pocket pool that it boggled the mind.
- Have no talks on Friday. Poor Nick Saban, although I don’t think he cared as long as he got paid.
- The educational sessions always seem to be better in title than they actually are. Not sure how to fix that other than move the submission date closer to the conference.
- Never do in Orlando. Too long and hard on the feet.
- The quality of the presentations. There needs to be more peer review of the content, perhaps fewer sessions with better content.
- Maybe a structured vendor list by hospital size. As my facility is a rural hospital, we are not going to take on new shiny object, but rather looking to optimize what we have an improve our current operations.
- Unlike other years, the lunch at the informatics symposium was disappointing. There was no coffee or refreshments later in the day, and it was very cold inside.
- There are not enough chairs, and we need bigger rooms for presentations and on the floor. Lots of standing.
- I had trouble with the app and loading sessions. Not all sessions were in the book, which was confusing. Because of this, I missed keynotes. Also, the app’s informatics filters were missing, so I could not easily find sessions I wanted to attend or specific vendor products.
- Speakers and panel discussions. Very little diversity in people and perspectives, seems to reflect the current leadership.
- Being bombarded by the same HIMSS “influencers.”
- Healthier food options or built in like VIVE would be nice.
- Stale content in sessions – seems to be the same topics and people reshuffled.
- Never use Orlando again. Ever. Worst location possible for HIMSS or any conference for that matter.
- Is still often difficult to stay focused on a booth presentation when a neighboring booth is using their sound system to reach a larger crowd. Maybe we should offer presentation audio via Bluetooth so we can actually hear the presenter.
- The traffic in Orlando is a nightmare. Taking the buses or Uber resulted in some long delays in reaching the convention center.
- I’d like HIMSS to condense the show floor when it doesn’t sell out. The Federal Government conference area was so far off the show floor it was difficult to get to. Once they didn’t sell the west end of the show floor, they could have moved things closer together.
- Better, healthier, and faster food options.
- More relevant keynote speakers, shorter exhibition hall hours.
- Bring HIMSS into the 21st century. Better formats, better lectures.
- Conference apps and networking lack other shows. It looks like only around 1,600 people opted in for connecting / messaging, while ViVE had almost 4,800, and I assume HIMSS has significantly more attendees.
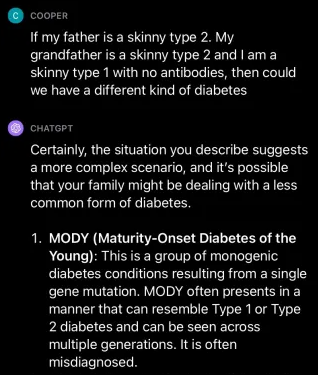
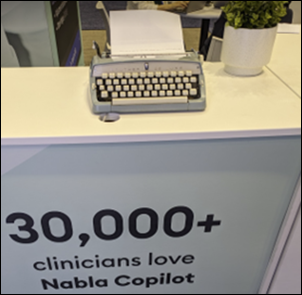
- More depth and practical applications of AI. The entire conference and showroom were focused on AI, but there was no real meat to the conversations, mostly that it’s new, we need to take advantage of it, we should be careful, need to use it responsibly – words without meaning. As physicians, we’re used to new tools and new drugs, for example, and I think this mindset helps us to better embrace AI, even accepting what we don’t understand. Additionally, adding salt to the wound, were folks claiming their product used AI, when it was a simple calculation or formula without any ML.
- Nothing. It will be my last after 20+ years.
- More reasonable food options cost-wise. Would like to see this smaller conference consider other venues such as New Orleans or San Diego because I bet it would fit now. I hate Orlando.
- There seemed to be blatant influence (paid) by big vendors doing “educational sessions” that were complete company product promotions, roadmaps with no third party or customer involved. Oracle Health was the worst! Other agenda items had good titles, but turned out invite-only, which drastically cut down options. As a person who has worked hard for years getting speakers on the agenda, something definitely seemed way off and commercially influenced.
- The HIMSS police called us out multiple times for overspill of our very expensive booth, but the anchor vendors did not get the same treatment. Surprise!
- HIMSS has completely lost touch with the provider community.
- More time between educational sessions. All sessions should be the same duration. Maybe after the first day, every session doesn’t need the intro about handout and eval in the app.
- More free food and drinks.
- Even less people.
- I did not like the keynotes. I think we need more healthcare people – yes, we had some, like the CEO of Hackensack Meridian – but I was not interested at all in Nick Saban, and granted it was Friday (so most people left), you might have gotten more to stay if you had a big name healthcare exec speaking then— Judy Faulkner, John Halamka, etc.
- Better process for main stage. Feel like much of core content is in interop showcase and not on main stages
- I ended up in a number of panel discussions. It’s good for different viewpoints, but I’m not sure that the format appeals to all subjects. I felt that some missed the main point/topic.
- Buy sessions too far removed.
- Floor on the far ends was a train wreck.
- Attempt at being cool on social media was cringeworthy. They need to figure out their lane, stay in it, and stop copying VIVE and their other event HLTH. They did it all first — puppy park, massage, stages on floor etc. It was not a good look.
- More subspecialty educational content. We’re an imaging IT company and there’s almost no relevant content to further attract the tribe of imaging IT professionals. This contrasts to the recent past, where there were always a handful of specialty talks to draw attendees.
- Continue the idea of co-locating vendors.
- Better food options and having it in different venue city rather than Orlando, Vegas, or Chicago if possible.
- The infrastructure in Orlando is terrible. Who planned this conference during spring break? It was pretty much impossible to get anywhere or meet anyone in a timely fashion, and the service at restaurant and other locations was slow and terrible. This conference cannot be held in Orlando any more.
For those who attended both HIMSS and ViVE, how would you compare the two?
- There was definitely more enterprise and implementation focus at HIMSS vs. ViVE’s partnerships and BD flavor with startups. More IT crowd at HIMSS vs. predominantly digital and innovation / investment crowd at ViVE. However, while ViVE has started bringing in CHIME crowd into its fold, HIMSS is increasingly becoming distant to innovation community.
- I like that I don’t have to bother about finding food at ViVE.
- ViVE in LA was just awful. Nashville was better. ViVe is trying to hard be too hip and let’s just forget the CHIME attendees actually visiting the floor except to get awards.
- VIVE resembles the HIMSS of years ago, before it decided HIMSS could be everything to every industry and needed a former vendor to be the Leader of the Pack.
- More entertainment.
- ViVE will replace HIMSS in the next three years. HIMSS has lost its appeal to me, I have been attending for 13 years, I am ready for a change, and ViVE is a refreshing change.
- This year’s ViVE in LA sux.
- Both have different value. I do feel that many of the hospital CIOs did not attend HIMSS24.
- Different energy and scale. HIMSS is bigger, ViVE is more personal.
- ViVE had much better vendors.
- ViVE makes the experience better as an attendee by providing food, drinks, and entertainment. However, from a work/business perspective, HIMSS is still the better show, and it’s not particularly close. There are just more people, more buzz, more product debuts, etc. ViVE is just a party.
- ViVE is far friendlier and feels less formal than HIMSS. It’s easier to see various speakers at ViVE with many of them right on the show floor. Included food and drink is also a nice touch that gives ViVE a relaxed atmosphere. HIMSS is the button-down business conference of yesteryear while ViVE tries to market themselves more like a music festival (with mixed results).
- They way they handle meals/food is so different. ViVE: Coffee stands and food spread throughout the exhibit hall, allowing many opportunities for networking. It’s very easy to grab something to eat or drink (which is built into the conference fees). Plenty of tables/spaces to grab a seat and meet others while getting something to eat. HIMSS: Coffee is $5+ and you need to wait in line in the hallway. Food is expensive and poor quality, typically far away from the events. You need to spend a bunch of time in line, then if you’re lucky you get a table but there’s a good chance you’re sitting on the floor in a hallway.
- ViVE is significantly better.
- ViVE is better. CIOs prefer it, so the power is shifting.
- Both are expensive and do not have the patient in mind. They’re both a money grab.
- They are very different conferences. At HIMSS, you have the advantage of having IT directors and clinicians (nurses and docs) talking about projects they did which, if you are CMIO/CNIO, might really help you as you work on your day to day issues. Yes, HIMSS has the tech companies, but it’s not the only group there. Also, the government track/ area at HIMSS had excellent presentations, but it was so far away (Hall F) if you were in another session you had to race, as most of these government presentations were only 30-minute “bursts” (but really good). ViVE was good too, but it’s really more tech people, companies, innovations, less clinicians (IMO). Yes. some government folks at ViVE, but not nearly as many. I think both are good meetings, but ViVE is SO expensive (the registration fee) that many groups, including mine, won’t send people. I only went as I was a speaker and got free registration.
- ViVE is spot on for the relationships I need to foster and HIMSS is where I go to partner with vendors or meet a bigger cross section of a customers.
- ViVE has grown, audience has evolved, and is for C-suite looking to make a difference and do business. HIMSS seemed much more mid-level in terms of the attendees. Different leagues. I will send a few (very few) from my team to HIMSS next year and my leadership team to ViVE.
- ViVE had more investors, HIMSS very very few. ViVE is more of a C-suite crowd.
Comments
- I miss HIStalkapalooza. The after-hours receptions hosted by vendors were a mixed bag.
- I was particularly disappointed to see a heavily inebriated vendor CEO (a serial entrepreneur, no less) behave very badly with a former health system executive at a networking event, berating them publicly for not giving business to the company while being employed. It was such an unfortunate event to witness and unacceptable behavior by any measure. Vendors need to understand that “No” and “Not Now” are perfectly good answers in current fiscal climate and that business decisions aren’t driven by individual event attendance but rather through stakeholder consensus in matrixed organizations.
- Having two shows so close to each other and SO similar is just a waste of limited resources for vendors and providers. Do we need one, let alone two?
- CHIME and its “leadership” have completely lost their way and ruined it. They don’t realize more people are actually laughing at them vs. looking up to them for guidance. Someone said to me they are more like ET (Entertainment Tonight) vs. 60 Minutes or BBC News. John Glaser must be sad to see what they have turned it into. Parties in Russ’s rooms, lavish all expenses paid board off-sites, international travel. Can someone say 503c3? cough cough audit? My company has more oversight on expenses!
- Both events took place while the US suffered arguably its worst cyberattack that directly impacted patient care. What did both organizations do to help educate? Why, they gave away even more trophies to each other, of course. Sad, frustrating, and vendors should demand an accounting of the foolishness taking place
- Based on what I spent to attend, I no longer think it’s worth attending.
- The people pic animes at ViVE are creepy.
- Being in Vegas back to back again, I might sit out next year.
- The overall feedback I heard from other attendees was that HIMSS was still where the “real” conversations were happening and VIVE was still more about the glitz and VC, aside from the CHIME Forum. There seems to be room for both, but it would be better if they weren’t so close together.
- I generally enjoy these conferences, but this year it just didn’t feel right. I think I’m getting too old (LOL).
- Would love to attend both HIMSS and ViVE, but simply cannot afford ViVE. It is above the limits of what my company will allow.
- AI seems to have given HIMSS a new life. Lots of serious and thoughtful discussions on how to find a way forward with this new technology!
- Other than reconnecting with peers from past conferences, HIMSS continues to struggle. Education sessions are stale. It’s more of a vendor conference. After more than 15 years of attending, I’m not sure I will continue attending. And I still miss HISTALKAPALOOZA. 🙂
- When do we move back to patients at the center of innovation, not PE, AI? Meanwhile, huge orgs cannot secure patient data.
- Likely to skip HIMSS because it is in Vegas. That is a negative, I think for many people.
- Conference has outgrown Orlando.
- Whatever opinion is on business model, HIMSS delivers people that want to connect either to see what is really going on vs hype, meetings with prospects, partners, and clients. As humans, we can filter out the BS. Foot traffic and talk tracks show quickly what is real and what isn’t. The AI hype, robot demos, and VR headsets are still more concept than actual real world applications. It seems like HIMSS HIT community is finally getting data quality matters.
- I left after a day and a half. Content was average and floor was much smaller. All in all an OK event, but not what it used to be. Good luck to Informa. They will need it.




































RE: Change HC/RansomHub, now that the data is for sale, what is the federal govt. or DOD doing to protect…