Paula Scariati, DO, MPH, MS is a physician informaticist, EHR governance consultant, and author of the book “EHR Governance: A Practical Guide to User Centric, Consensus Driven Optimization.”


Tell me about yourself and what you do.
I’m an preventive medicine and public health doctor. I fell in love with the promise of what technology could do to make patient care and access better, so much so that I left the private practice that I had in San Diego 15 years ago to formally retrain in informatics.
But nothing that I learned in my academic studies really prepared me for my first job as a physician informaticist in a large, enterprise healthcare system. Providers were frustrated by poorly designed software, inefficient workflows, and low-value tasks. EHR governance was immature, and was often driven by well-meaning executives who didn’t really use the EHR. End-user requests were low priority and frequently lost to follow up.
In short, the processes were slow, poorly coordinated, and had lots of bumps, detours, and do-overs. It was intense. The tipping point came when a large region that was part of the enterprise threatened to return to paper, and there was a crisis. Out of that crisis, a methodical, user-centric, Agile approach to EHR governance was born.
How has EHR governance changed now that most health systems have chosen and implemented an EHR?
Governance has matured organically over time. In the beginning, back when most organizations went live, it usually meant that a process was stood up at the end of go-live, where that critical mass of requests that were made during go-live, but not necessarily addressed during go-live, were handed over into a queue. That was the focus of early governance work, the robust adoption of a new system with well -integrated workflows.
But once those I’s were dotted and T’s were crossed, the focus of governance then shifted to optimization. That work included end users adopting new tools and refining interfaces. This organization was looking for more effective, efficient care. It took probably several years for that to unfold.
Then the organization moved on to the next phase of EHR governance, which I call transformation. It’s at that point where the organization’s governance framework would be well established and trusted. It has become part of the cultural norm of organization. There’s now a pathway, hopefully an Agile pathway, for conducting pilots or proof of concepts, which allows the organizations to quickly vet new technologies, modules, and features. There’s also an established system for communicating and socializing change.
I’d like to believe that over these last 15 years, many organizations have found a level of transformational maturity in their EHR governance processes that works well for their healthcare system and their culture. However, I’ve also spoken with so many leaders and organizations where EHR governance never got a strong footing, or where well-designed governance processes were fouled by mergers and acquisitions or major leadership changes.
Do health systems incorporate the participation of medical staff technology naysayers in addition to the “friendlies” who will reliably support most executive decisions?
EHR governance needs to be led, and it needs to be led by somebody who is well respected and has the power to make changes when they need to. That right person needs to be embedded in a consensus-driven governance process. That process needs to listen closely to everybody. People who say they’re doing a good job, but especially the people who tell them that they are not.
Sometimes that negative feedback is more representative of the truth. Sometimes it isn’t representative at all, but it’s the canary in the coal mine, meaning that that person has the unique ability to see a real problem before others do. Occasionally, it might be a disruptor who has a less-than-kind intention, who can in good faith be ignored.
But it is important to remember that a solid EHR governance structure is a two-way street. Communication goes out, but communication also comes back in. You need to be listening to the voice of the end user. Because when that is done well, a responsive governance process can throttle and balance an organization between that need for change and that problem with inertia or the status quo. Every organization has a different level of tolerance. A good system will recognize that and reduce the amount of fatigue and burnout that an organization will have because it is keeping to close on what’s going on.
Early EHR decisions were often made without thorough physician involvement, or by departments that wanted to make their own jobs easier by using the EHR to push more work onto physicians. Are some of those decisions being revisited or are physicians being asked directly how the EHR hurts or could help their work?
I think it’s safe to say that every organization that adopted an EHR back in 2009, which is when HITECH was enacted ,would have been thrilled if the software was mature and user friendly. But we have to remember that every vendor’s core EHR product was initially designed to meet Meaningful Use metrics, and that went on for seven years. Nowhere in there was a mandate for the user interface to be friendly or for the user experience to good.
That exists even today. Our former Meaningful Use metrics have now morphed into the Promoting Interoperability Programs and eCQMs. This is all the basis for driving value-based care, but it took a number of years for that emerging body of literature on the unintended consequences of EHRs, note bloat, provider fatigue, and burnout to elevate the importance of the end-user experience and push it to the forefront. Physicians were rightfully frustrated and local decisions were made, decisions were made by the vendors, but they weren’t made with the idea of how to improve the user experience. They were made, how do we meet this metric? How do make this quality metric or safety metric get reported so that we can obtain Meaningful Use dollars?
There was also a lot of frustration on the part of physicians because they were now being asked to play well with others in the sandbox. They were asked work with their colleagues and other teams to come to a consensus on how to design their user interfaces and workflows. This was a difficult task for some specialties, such as cardiothoracic surgeons who might be used to having their own unique way of doing things. This is where having fair, transparent, equitable governance processes is incredibly helpful. It levels the playing field and it sets consistent expectations.
Physicians are just about the only professionals who are expected to enter data into a computer system while doing their jobs, and often the data that they are recording doesn’t benefit them or their patient directly. Is AI or the use of scribes likely to change that?
Forcing physicians to become data entry clerks has been one of the greatest failings of EHR adoption process being driven by Meaningful Use. AI will get the keyboard off the physician’s lap, which will go a long way toward restoring the doctor-patient relationship. In fact, the highlight of HIMSS24 was the latest iteration of ambient voice technology married to artificial intelligence. These types of software capture the doctor-patient encounter verbatim and then use AI -driven logic to digest that information into a succinct, readable node. It’s amazing, and I think it’s just the beginning of what AI that is thoughtfully utilized in healthcare can do.
However, there’s a lot of pressure on AI to solve all the problems that we have. It would be very nice if it can do that. I’m waiting and hoping that that will be the case. Some people say five years. I am a big fan of following Eric Topol’s voice in the matter, and I think he’s more optimistic than most in terms of how quickly this will unfold. But either way, I think it’s going to go a long way to help correct a lot of the problems that we’ve encountered as a result of how our initial work with EHRs has happened over the last 15 years.
How does the art of medicine coexist with the use of technology to standardize processes and guide medical decision-making?
When we first started digitizing medical records, a good deal of folly took what was on paper and just made it digital. We didn’t really use the knowledge that we had of how to make the EHR better, stronger, and faster than paper ever could be. But now, we see that the science underlying medicine grows exponentially every day. Just look how much medical literature is published each day. Then there’s the patient’s genomic data and now their phenomic data and so much more. It is absolutely impossible for any one provider or provider team to keep pace without using electronic tools that can securely capture, store, and make some good sense of it all.
What I see on the horizon is that good clinical decision support tools and analytics are going to expand the horizon of the physician. But the road to getting there is going be bumpy. We haven’t really taught our physicians or given them tools in a way that are user friendly. That’s where governance comes in, helping us to figure out how much we can change, how quickly we change, and vetting stuff ahead of time so that we determine what kinds of problems it may have and then deploy it using that group of early adopters who likes to do that type of initial pilot or proof of concept work, and help them to become the agents of change within our organizations.
Epic’s implementation model involves a rigid methodology and the assumption that C-level hospital executives will follow the recommendations of vendor employees who might have been sitting in a college classroom a year or two before. Did that level of prescriptive vendor involvement change the way that hospitals implement technology?
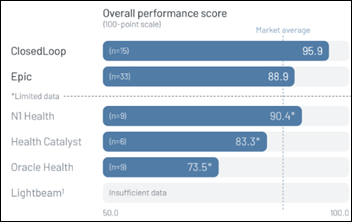
I gave a talk yesterday and user experience with Epic.The takeaway is simple — incentivized behavior change is more effective, and Epic was very smart. Early on, they recognized that organizations didn’t know what they didn’t know, and so they led. They were prescriptive. They trained and deployed resources. They didn’t nickel and dime their customers, but the level of support that came with them had a larger price tag and, in the end, better customer satisfaction. I’ve spoken with a number of organizational leaders that have used Epic and other EHRs, and they consistently they tell me that they find the Epic model to offer added value.
The takeaway is that incentivizing behavior change, being prescriptive — especially in an environment where people are learning something new, where they don’t know what they don t know — is a valuable way to deploy something.
Is governance different in Epic-using health systems, either because they are self-selected as large, academic medical centers or because they are influenced by Epic or its other customers?
Epic had its origins in the ambulatory world. A number of Epic installations are organizations that have brought together large groups of ambulatory providers. We used to call the ambulatory world the wild, wild West, because in the inpatient world, a large, complex go-live has a lot of moving parts, while the ambulatory world, each individual practice has its own way of doing things. When you try to bring that together under a governance structure, it’s a little bit more challenging to get people to talk to each other or get them to agree on a certain interface or workflow.
In my experience, maybe not in everybody’s experience, taking the time to draw on a group of leaders to represent a specific region or practice and bringing them together to drive the change that you call governance is critical.
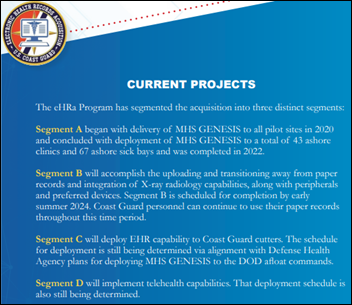
Another good example of that is watching what is happening now with the go-live for the VA. Very, very bold. They are trying to have the whole VA system and the Department of Defense be on a single instance of Oracle. That’s a bold undertaking from a governance perspective, in terms of having everybody work together and use that same platform in a similar fashion.
Implementation of AI is more of a blank slate than bringing up an EHR since health systems can set up just about any logic and workflow they want, good or bad. How will AI governance work?
I wouldn’t necessarily say that we have a blank slate today. We’ve now been through over a decade, almost 15 years following HITECH, of doing EHRs. Some organizations have been on that same EHR, while others have gone through a second go-live with another EHR. Some have gone through mergers and acquisitions.
What I see, and what I keep hearing from the different organizations that I speak with, is that physicians and other healthcare providers and users are tired of that “unlearn something old, learn something new” unlearn-relearn technology cycle that we’ve entangled our healthcare providers in. Our human nature is more inclined towards inertia and the status quo than it is to these iterative cycles of rapid change. For example, I may offer a physician a better, more efficient way to do something, but it’s not that unusual for them to decline, saying they would rather keep their current process and workflow even if it is broken.
I see what’s coming forward with AI as incredible. It’s going to be another technical revolution. But I’m concerned that we now have a large amount of change fatigue, and in some cases burnout, from all of the change that we have been throwing at providers for the last decade and a half. They predict that the way we practice medicine will completely change in the next five years, and that is both exciting and frightening. But solid AI governance processes are the key to helping organizations throttle how they unfold that technology so that we have a legacy of innovation and equity, not burnout and the dissolution of the doctor-patient relationship.
More physicians on the medical staff are employed directly by health systems now instead of being based in the community or contracted through an external company. How has that affected the integration of physicians into technology decisions or their ongoing technology training?
I always found that group of community-based doctors to be an outlier in how we handled them during our lives. Their office often used a different EHR than the one in the hospital where they worked. It wasn’t a given that you would automatically just bring them up in their practice on the same EHR. They would use some sort of interface in their office to be able to use their office-based EHR that was interfaced to the hospital EHR. That was a clunky way of thinking about things, and something that I really had wish we had been more forward thinking about in terms of continuity of care across the continuum of care in medicine.
I would not say that it’s a big difference in terms of how we engage with them. Often they were powerful because they brought lot of money into the organization, so there was a high level of sensitivity to making sure that their EHR worked well for them. But engaging them in governance and in consensus was the same as it was for any other group. Again, with that added caveat that when we were looking at workflows, it was the hospital-based workflows and not necessarily how it would always work for their EHRs within their office. But we often would go out and do a visit into their offices just to make sure that there was something that was working well and that it wasn’t double entry, or that something was inclined to making more errors than not.
How do you see the role of the CMIO changing?
I am hopeful that CMIOs over the last decade and a half have shown that they are strong leaders. I would love to see them elevated from what is oftentimes a “small C” in the organization to a “large C,” where they have a seat at the table with the CEO, CMO, and CIO. They do in some organizations, and some they don’t. But there has been recognition of the expertise that they bring to the table, as well as an evolution in what the CMIO is expected to be able to do, that has caused that role to be elevated to a higher level.
As we move towards more AI -driven technological revolution in healthcare, that voice, that person, and that expertise is going to be critical. Over time, roles have been renamed. They have become the chief digital officer or chief AI officer. It may go that way instead of just changing the world of the CMIO to embrace a broader swath of what is technology. They may create these other roles that are more specialized. Either way, the CMIO has been elevated in stature and importance within every organization that is seeing just how much technology touches every aspect of healthcare.



































Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…