News 12/8/23
Top News

Providence will sell its Acclara revenue cycle management company to R1 RCM for $675 million in cash, warrants to purchase $135 million worth of R1 shares, and a 10-year contract to receive revenue cycle management services from R1.
R1 shares, which are up 11% in the past 12 months versus the S&P 500’s 16% rise, rose slightly on the news, valuing the company at $4.7 billion.
Reader Comments
From Green Slime: “Re: award. See this LinkedIn post about another vanity award.” Dayton Children’s CIO J.D. Whitlock is tongue-in-cheek proud to be nominated for “Most Pioneering Magnetic Leader Revamping The Healthcare, 2024,” which he can win by paying $2,800. I found a back issue from issuer The CIO World, which is full of grammatical errors and odd wording that makes it obvious that its editorial terroir is not nearby. It describes itself as “an archway that caters to Entrepreneurs’ quench of technology and business updates.” Still, what they are doing is legal and in fact is perhaps the perfect business – selling vanity strokes to folks who crave them, even those who work in The Healthcare. The downside is that you look like a loser when you’re caught bragging on an obvious pay-for-play award.
HIStalk Announcements and Requests
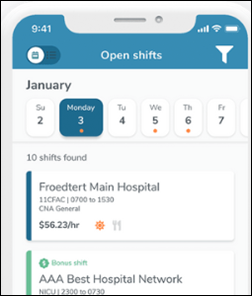
Welcome to new HIStalk Platinum Sponsor SnapCare.SnapCare is an AI-enabled workforce marketplace that serves the entire continuum of care. Its platform offers healthcare facilities complete visibility into the ideal talent mix for their unique needs and associated costs. The company designed its workforce solutions to significantly improve client savings and efficiencies, minimizing the need for intermediate agencies, returning control to healthcare facilities, and ensuring total transparency in pay and pricing. Its pioneering technology and comprehensive staffing services offer a smarter way for facilities to manage their workforce needs and deliver quality patient care. Thanks to SnapCare for supporting HIStalk.
I found this SnapCare explainer video on YouTube.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
Novant Health will outsource some of its IT department’s work to India-based Wipro, but declines to say how many positions will be affected.
People

Industry long-timer Brent Dover (Kalderos) joins AI-powered clinical data management technology vendor Carta Healthcare as CEO.

William O’Toole, JD (O’Toole Law Group) joins DrFirst as counsel.

Fortified Health Security hires Greg Breetz, Jr. (Valera Health) as CFO.

Sarah Jones, MBA (Firefly Health) joins B.well Connected Health as chief outcomes officer.
Announcements and Implementations
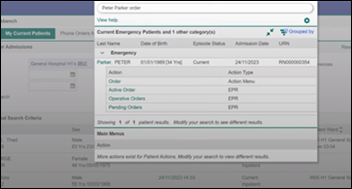
InterSystems announces GA of TrakCare Assistant, a search-based navigation tool for its TrakCare EHR. Internal testing shows that Assistant reduces EHR interaction time by up to 66%.
In Canada, Fraser Health will pilot the use of Google Cloud’s generative AI to help create clinical documentation in Meditech Expanse.
Three-fourths of ambulatory care physician leaders who were surveyed by WellSky say that their organizations don’t have relationships with post-acute care providers, and most referrals to them are sent by fax or telephone. Most respondents expect their participation in value-based care programs to increase, while more than half of those surveyed say they don’t participate in Medicare’s Transitional Care Management because of shortages of staff, data, or technology.
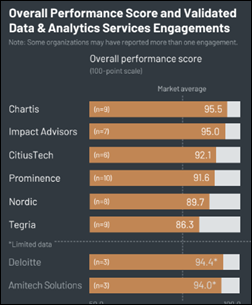
A new KLAS report on data and analytics services lists Chartis, CitiusTech, Impact Advisors, and Prominence as being broadly validated across four disciplines – advisory consulting, technology services, operations improvement consulting, and managed services.
Privacy and Security
HHS lays out its plan to improve cybersecurity in healthcare, which includes setting healthcare organization performance goals, providing financial incentives for implementing cybersecurity practices, and enforcing cybersecurity standards within Medicare, Medicaid, and HIPAA.
Epic raises concerns about an ONC proposal that would require EHR vendors and HIEs to remove reproductive health information from data-sharing programs upon patient request. Epic says that the proposal would increase clinician documentation burden and is not technologically feasible, while a family doctor observes, “EHRs have been working so hard to share data automatically that we’re now behind in thinking about how to not share when that data can be used to criminalize a patient.” Proponents say that patients and providers could be charged with felonies in states where abortion is illegal if information from abortion-legal states is shared across state lines.
Washington University (MO) sues the state’s attorney general over his demand for access to patient records from its transgender center, which he is seeking under a consumer protection law that addresses false advertising. The AG’s office says it is entitled to information about treatment, referrals, prescriptions, and compliance with standards of care, while the university says that HIPAA pre-empts state law and allows disclosure of PHI only to a “health oversight agency.”
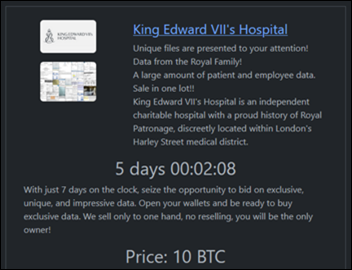
Security researchers report that a security flaw in the DICOM medical imaging standard has caused millions of patient images and exam notes to be exposed to the Internet. The affected servers, most of them hosted in the cloud either did not have security measures enabled or used weak authorization.
Other
Ardent Health Services restores access to Epic after nearly two weeks of downtime following a November 23 cyberattack.

The local paper profiles Jonathan Hatfield, who graduated college with a degree in bible studies, became a night shift janitor at Klickitat Valley Health (WA), taught himself IT, started the hospital’s IT department, was assigned responsibility over other departments, and then was chosen to be CEO of the hospital.
Sponsor Updates
- Black Book Research outsourcing services survey respondents recognize Dimensional Insight as the top outsourced analytics solution.
- First Databank’s FDB Vela e-prescribing network earns HITRUST risk-based, two-year certified status.
- Mobile Heartbeat announces that its cloud-based clinical communication and collaboration solution, Banyan, is now available on the Microsoft Azure Marketplace.
- Healthcare Growth Partners publishes a snapshot of the radiology software landscape, 2019-2023.
- KLAS Research recognizes Impact Advisors as a top provider of data and analytics services in its Data & Analytics Services 2023 report.
- Medicomp Systems releases a new “Tell Me Where It Hurts” podcast featuring Bob Taylor, DO, chief product strategies of TouchWorks EHR, Altera Digital Health.
- Meditech Lead Designers Tammy Coutts and Michael Shonty describe their work to advance disability inclusion within EHRs and to update the HIMSS Electronic Health Record Association’s Personas Library to include accessibility in recent HIMSS EHRA blogs.
Blog Posts
- Smart Coverage Detection Equals Better Patient Care + Stronger Bottom Line (EClinicalWorks)
- “Living Positive” Film: a Community of Hope, Brought Together by HIV (Findhelp)
- 3 Ways to Optimize Automation in Revenue Cycle Management (FinThrive)
- Is Data Migration to the Cloud Inevitable? (Five9)
- Navigating incident response: Lessons from a hospital cyber attack (Fortified Health Security)
- 5 Reasons Why Consistent Health Education is Important (Healthwise)
- Leadership Through Service: Our 2023 Social Impact Report (Healthcare IT Leaders)
- Empowering maternal and newborn health research with Inovalon data (Inovalon)
- Streamlining EMR Interactions with a Reimagined User Experience (InterSystems)
- Hiding in Plain Sight: Leveraging Existing Patient Data for Early Detection of Diabetes (Lucem Health)
- 3 Tips for Surviving the Holiday Emergency Department Rush (Medhost)
- How Cloud Technology is Changing the Face of Clinical Communication (Mobile Heartbeat)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.























With McGraw’s new position at Transcarent, it seems like Glen Tullman might be getting the Allscripts band back together.