Readers Write: More Technology is Not Always Better in Specialty Medication Workflows
More Technology is Not Always Better in Specialty Medication Workflows
By Julia Regan
Julia Regan, MBA is founder and CEO of RxLightning of New Albany, IN.

Over the past decade, there has been a consistent promise made that technology would make provider and care team lives easier. However, the proliferation of EHRs, point solutions, manufacturer and vendor portals, and digital devices have made various processes not only more cumbersome, but more confusing and frustrating.
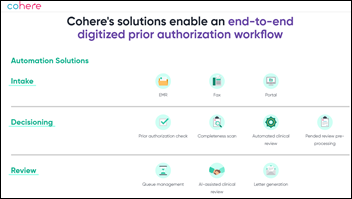
In specialty medication onboarding specifically, an HCP may need to visit upwards of 40 portals or websites throughout their day to check patient benefits, submit prior authorization, find and complete enrollment forms from various manufacturers, collect patient consent, and track enrollment statuses. It’s no wonder that healthcare is facing a burnout crisis.
As technology has become ubiquitous, it has created an additional challenge for biologic coordinators and medication access teams, especially those that work to support patients with complex treatment plans or work across therapeutic specialties. This, in turn, increases cognitive load, screen time, and clicks, slowing the completion of the necessary steps in a patient’s care journey and decreasing overall speed-to-therapy.
As an example of portal fatigue, a medication access team member at a large health system may need to support an oncology patient who is prescribed multiple brand name specialty medications, each of which requires portal access to obtain assistance. One of the drugs may have a manufacturer-sponsored co-pay assistance program, another may be eligible for foundation assistance, while another may need additional approvals via prior authorization. In order to effectively support this patient through their medication access journey, multiple portals and logins are required.
Instead of the common perspective that “more technology = better,” we must shift to a new perspective that says that “unified, purpose-built – even less – technology = better.” Instead of forcing teams to scour the web for up-to-date manufacturer forms, why not house all forms, and enable submission and delivery of those forms, in one solution? Instead of routing a form for patient and provider signatures via a distinct process, why not enable seamless signature collection at the point of care? Instead of manually researching affordability options — foundations, PAP, co-pay, etc. — on a variety of sites, why not integrate those options into the same portal where the forms and signatures live? Creating a uniform, digital entry point that leverages a repeatable process for any drug, any manufacturer, and any patient can significantly reduce cognitive load and burnout.
As I’ve had conversations with providers, care teams, and medication access specialists over the past few years, the more I’ve realized that “more technology ≠ better.” As patients enter and exit their offices, they wish for integrated, intuitive, secure technologies that minimize work and accelerate the speed at which they can deliver quality care. While the specialty medication onboarding process includes a variety of steps to help support patient access — benefit verification, PA, consent, financial assistance, and fulfillment — there is no reason that these steps cannot be automated, integrated, and fast. An HCP should not have to worry about which manufacturers may or may not have sponsored a program, or if the technology will work for a specific patient. To reduce burnout and create consistency, technology should work the same way every time.
It is up to clinical leads, IT teams, and other leaders to sound the alarm and support the launch of solutions that reduce burden and burnout for their teams, instead of those that create more work. A single digital entry point for any patient and any medication is a reality that is within reach. We just need to drive provider adoption of these tools. The only way we can ensure better, faster, more affordable care for patients is to help providers with the work they do every day.

















































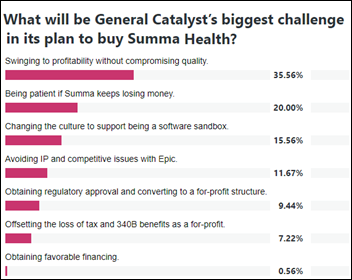

It is incredibly stressful once you leave the Epic center of gravity. I have spent my ex-epic career wondering if…