Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
EPtalk by Dr. Jayne 5/11/17
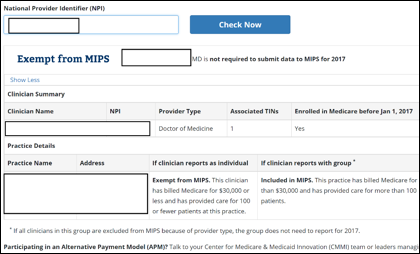
The CMS Quality Payment Program website has been updated with an “Am I included in MIPS?” feature. Providers and organizations can search by NPI (sorry, no bulk search feature for groups yet) to determine if they are included. The site also doesn’t flag whether you’re participating in an ACO, but rather tells you to talk to the leaders managing your participation.
Forbes posts an article about the Internet making us lose trust in our doctors. I think many of us agree (at least anecdotally) that things have changed over the last decade, and exponentially so after the rise of the smart phone. The piece details a study looking at whether screenshot content can prime a pediatric patient’s parents to be biased towards a particular diagnosis. When the physician diagnosis didn’t match the Internet diagnosis, parents were less likely to trust the physician diagnosis and were more likely to say they would seek a second opinion. The researchers’ conclusions note that “conflicting online information could in some cases delay necessary medical treatment. Physicians must be aware of the influence the internet may have on parents and ensure adequate parental education to address any possible concerns.”
Physicians in the patient care trenches have known this for a while, that it can take a significant amount of counseling and discussion to counteract what “Dr. Google” or a number of other websites may have said. When it’s the occasional patient arguing with you about your clinical expertise, it can be managed, but when it feels like every patient is coming in the door with a preconceived notion about what is going on, it is a direct contributor to physician burnout. I don’t believe physicians are omniscient or that our opinions should be absolute, but sometimes you just wish your patients would trust your decades of experience and the many dollars and hours you’ve expended to arrive at your level of clinical judgment. Even a seemingly straightforward diagnosis like “contact dermatitis due to plants” can suck time out of your day when you have to engage around smart phone photos of poison oak, ivy, and sumac. Bottom line is, it doesn’t matter what plant got you, we’re going to treat you the same way regardless of botanical factors and you need to avoid coming into contact again with whatever it was.
Sometimes it’s hard for people to understand what it’s like to be a physician and the pressures we’re under outside of dealing with payers, metrics, regulations, etc. I’m talking about the actual clinical pressure to be 100 percent accurate. If you’re a good physician, it weighs on you and it’s hard to keep in balance. I recently had a situation where a patient perceived a poor outcome based on my diagnosis. She had come to the urgent care on a Saturday with back pain, which had some distinct muscular features and no acute findings on an x-ray, and was diagnosed accordingly. Our practice always has a second reader for films, and my colleague agreed with my reading. The patient was instructed to follow up with an orthopedic specialist on Monday (two days from the visit) if she was not improving. She followed up, and the orthopedist sent her for advanced imaging and diagnosed a vertebral compression fracture, then performed an expensive procedure. She came back to us demanding compensation for our missed diagnosis.
Our standard practice in this case is to convene a peer review and to also have the films re-read by a radiologist, who also failed to appreciate the compression fracture. Peer review found my treatment to be appropriate given the history and exam and the setting (urgent care). The patient was given appropriate follow-up instructions and her pain was managed adequately. Of course, we don’t have access to the advanced imaging results showing the fracture, so it’s hard to tell whether the specialist is taking advantage of a marginal finding or whether something was really there. The patient’s treatment wasn’t even delayed by my supposed misdiagnosis since she would not have been able to have advanced imaging until Monday anyway due to her insurance and its requirements. Getting a pre-certification for a non-emergent ambulatory procedure on a Saturday just doesn’t happen in our world. Assuming you agree there was a fracture, she received definitive care in a timely fashion that was more impacted by the fact that she came to care on a weekend than it was by a potential misdiagnosis.
One also has to consider the role of the urgent care, which is to rule-out any life-threatening conditions and to provide treatment for illnesses and injuries that require immediate care. Sometimes we’re also just there for convenience, for patients who don’t want to wait to see their primary care physician or whose schedules don’t mesh with their primary physician’s office hours for refills on maintenance medications. There are numerous situations in which we do not provide definitive care. Most fractures are merely stabilized and then the patient is referred for orthopedic management. For most urgent care centers, anything requiring imaging that is more than a plan film x-ray has to be referred back to a primary physician to coordinate authorization, scheduling, and follow up. We’re not in the position to order complex studies and follow up on them, and most of the time we do strive to get you back to your primary care physician for follow up.
Even when a physician feels he or she has done the right thing, and their care has been validated by a peer review and supplemental evaluation of diagnostics, it still weighs on us. There is the nagging sensation that we should have done something different, and that the patient thinks we’re bad doctors. It’s hard for people outside our world to understand what that does to a person, and culturally it’s difficult for us to find people to talk with about our experiences. It’s also legally difficult, sometimes, when you think the patient is going to sue. We end up stuck with only the risk management team to talk with and they’re not exactly caring nurturers who want to help you work through the psychological ramifications of a poor outcome and subsequent lawsuit.
Keep this in mind next time you encounter a physician who seems aggravated and preoccupied. Or any health care providers, for that matter. We’re all walking around with some baggage, and sometimes a malfunctioning EHR or one more regulatory hurdle is all it takes to break us.

Email Dr. Jayne.


I am still trying to wrap my head around the idea that CMS would build a MIPS checker and not give some kind of ability to check at a group level. CMS’s response is that it is a privacy and security issue b/c TINs are tax IDs. Great! So let us upload a list of NPIs (leaving the onus of TINs off the table) and see if they qualify as a group based on the individual NPIs submitted. MIPS in the end encourages group reporting. Not having a tool to validate group reporting is less than useless (and how many providers will miss the caviet of ACO reporting tacked on the bottom of the page and think they are good to go?).