MACRA’s Marketing Problem
HIStalk digs into why provider awareness of MACRA is lacking and the likely impact it will have on their ability to stay in business.
By @JennHIStalk
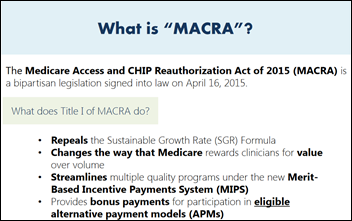
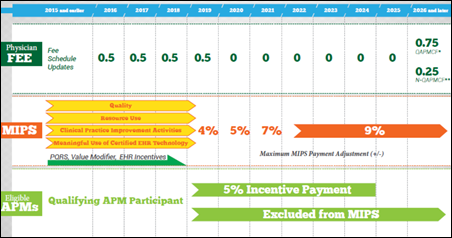
The Medicare Access & CHIP Reauthorization Act has seen its fair share of headlines since it was introduced just before HIMSS15. MACRA’s implications for patients and providers contributed to a lot of the show-floor buzz in Chicago that year, while conversations around its potential for payment reform heated up even more in Las Vegas at HIMSS16. The release of a 962-page proposed MACRA rule in April provided fodder for industry media outlets, and last week’s release of four “pick your pace” options ahead of a final rule have no doubt eased the anxiety of many physicians fretting over the January 1, 2017 start date.
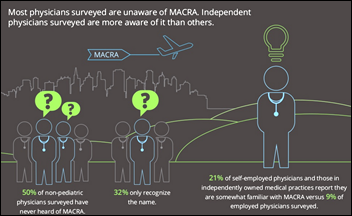
In short, it seems that MACRA has spent more than its fair share of time in the spotlight, leading many in the industry to assume that providers have been keeping up with its developments.
The results of a Deloitte survey of physicians on MACRA awareness and preparedness (conducted before the proposed rule was released) tell a very different story. Of the 600 primary care and specialty physicians surveyed, 50 percent admitted to having never heard of the legislation, while 32 percent knew it only by name. Independent physicians were more aware of it than employed MDs, though not by terribly much at 21 versus 9 percent.
Where does this unawareness stem from? Have providers become so accustomed to regulatory delays that they no longer pay attention until implementation is just weeks away? Has CMS, for lack of a better phrase, shot itself in the foot when it comes to introducing legislation that providers automatically assume is too cumbersome to digest and apt to be postponed numerous times?
Providers who have attempted to keep the lights on through Meaningful Use, ICD-10, and now MACRA surely can’t be blamed for not keeping up with the latest reforms issued from on high. Or can they?
Too Busy to Take Notice

“It’s not only physicians who have a lack of awareness,” explains Mitch Morris, MD, vice chair and a US global sector leader at Deloitte. “It really snuck up on the industry in general. Even now when we go in and do a briefing in the executive offices of a health system or payer, they say, ‘Wow, I didn’t realize all of that was in MACRA.’ It’s not very well understood. Unlike in the ACA, which had lots of publicity and everyone was dissecting it from Day 1, MACRA was thoroughly bipartisan and didn’t get a lot of [mainstream] publicity. The medical trade associations, the usual source of news for providers, just haven’t really been pushing this. On the surface, it sounds like a boring topic, but as you peel away the layers, you realize it’s going to be very impactful.”

AMA Immediate Past President and emergency department medical director Steven Stack, MD says Deloitte’s findings line up with the association’s own from its physician focus groups. “I think the upcoming changes are difficult for many to absorb while they are fully engaged in the day-to-day work of their practices,” he says. “And, keep in mind that when the legislation was enacted in April 2015, physicians were told the new system would not be implemented until 2019. They had good reason to believe there was no hurry for them to get up to speed.”
“Finally, it is simply not possible for the AMA or anyone else to begin broadly disseminating detailed educational material until the final regulation is issued,” Stack says. “We have been developing resources intended to help physicians get ready, but really all they want to know is what the rules are. We just don’t have all the information yet.”

Physicians working in the trenches of day-to-day care echo Stack’s observations. “I think most physicians would agree that the best use of their time and skill would be to simply treat patients and stop worrying about the endless administrative tasks of medical practice,” says Scott Mayer, MD, director of quality control at Today Clinic (OK). “Time to practice the art of medicine sounds so nice, but the reality is that being a physician these days requires so much time be spent outside of patient care that it has become increasingly difficult to keep up with so many changes in healthcare.”
“Patients need treatment now,” he emphasizes, “so unless a policy takes effect immediately, a lot of physicians don’t want to deal with it until it is absolutely necessary. I also suspect that many these days here the word ‘change’ and snort in disdain at the thought of something else that will further complicate their ability to practice medicine.”
University Physicians Group (NY) Medical Director and Aprima Chief Medical Officer Jeffrey Hyman, MD adds that lack of MACRA awareness on the part of employed physicians may stem more from the fact that once a physician is employed, the ‘business’ of running a practice becomes akin to background noise, outranked by patient care. “As an independent,” he adds, “you still have to worry about every issue of the practice of medicine to be successful and so attention is paid to every last detail.”
Today’s Diversions Trump Tomorrow’s Regulations
The details diverting the attention of physicians away from MACRA preparation are numerous and probably well known to HIStalk readers. “For physicians in private practice,” says Mayer, “a considerable amount of attention, resources, and stress are focused on just getting paid for the services they provide. Decreasing reimbursement rates, more regulations, more paperwork, and the increasing costs of maintaining a profitable medical practice are sure to distract a lot of us. We are wondering what the future of medicine looks like while doing our best to provide quality care now, find joy in our work, and avoid burnout.”
Hyman puts burnout at the top of his diversion list, too. “It’s a big deal these days,” he emphasizes, “and non-physicians have difficulty with this concept. Treating patients takes a great deal of concentration on details of their histories and physical findings, ordering lab and radiology tests, and then putting all these facts together and coming up with a successful treatment plan. Also, the need to think about formularies, getting pre-authorizations, and dealing with call-backs, admissions, and labs coming in … and don’t forget the EHR and all of its messages coming in at a furious pace. It takes a great deal of attention and MACRA, when read, sounds like a future issue. It just seems distant.”
Hyman’s observations on EHR-related physician burnout, while nothing new, seem to continually be backed up by studies large and small. A prime example is an AMA-sponsored time and motion study released last week that found ambulatory practice physicians spend almost twice as much time working on the EHR or performing other desk tasks as seeing patients. Observed MDs spent only 27 percent of their available time in face-to-face interactions with patients.
The results aren’t surprising to Morris, who notes that for the third year in a row of Deloitte’s research, three out of four physicians will answer that EHRs take too much of their time and cost too much money. “As an industry, we still have a long way to go so that they feel they add value. We’re not where we should be with the vision of EHRs.”
Morris is quick to add that no matter their employed or independent status, the time and attention of physicians are increasingly spent dealing with tremendous reimbursement pressures. “There’s a lot of pressure to move from volume to value-based payment systems,” he explains, “where part of their income is placed at risk. That pressure has many physicians very, very anxious and, to some degree, angry. They’re not always sure who to be angry with, but they’re not happy about the situation that they’re in. Even though the economy has recovered and there’s more discretionary spending, there’s still a lot of screws being turned down on physician incomes.”
Passing the Buck
Morris brings up a good point with regard to the slow boil of physician’s anger at being put in a position that leaves them little time with patients and even less to deal with impending regulations like MACRA. It could be argued that numerous entities should be on the receiving end of that emotion – CMS, payers, trade groups, and vendors – even patients and physicians. Fingers will likely start pointing to these same groups once MACRA hits, no matter the chosen start date, and physicians realize they’re out of time and unprepared.

“The industry has the obligation to educate and provide reasonable technology, tools, processes, and training to physicians to assist in the change management of MACRA,” says Kareo CMIO Tom Giannulli, MD, MS. “Those entities that contract with physicians should be very clear as to how their contracts will change. This includes CMS, which unfortunately does not communicate as well with physicians as they could, and based on their historical record, their deadlines are generally not respected. I would like to see them set up a website and online education program that requires each MACRA-participating physician to sign in and complete a half-day course on tech, tools, process, and regulation in order to continue their Medicare billing at full rate. There are a lot of other groups that have and can share a viewpoint, but those they contract with are the right source of information.”
Stack also feels that, while everyone has a role to play, CMS needs to reach out to provide simple tools and procedures to help physicians succeed. “They must strengthen their help lines and educate their staff so they can provide accurate information,” he adds. “CMS should also conduct train-the-trainer sessions and provide much more support to specialty societies to help them answer questions of particular interest to their members. Organizations like the AMA, state medical societies, and national physician groups can be very helpful by tailoring complex material more to the needs of their own members. Specialties, for example, can highlight quality reporting and CPIA activities that are most relevant to their audience, and so greatly simplify the learning process.”
“Employed physicians will likely be spared some of the specific tasks,” he adds, “and the need to be mindful of all the reporting deadlines, but there’s no doubt they will still encounter workflow and documentation issues.”
Hyman looks for MACRA guidance from Northwell’s dedicated group of staff already dealing with these issues and, as one would expect, UPG’s EHR vendor. “Aprima is also coding a great deal of information into their program to assist their doctors in getting this done successfully,” he adds.
Getting Started (but Preparing for Delay)
Hyman and his colleagues have been preparing for MACRA since it was first announced in 2015. “Our group of analysts, the Incentive Team , has begun the teaching process,” he says, “and we will interface between our physicians and the rules so it gets done in the most efficient way for our doctors. We will be ready with our team approach and help from our vendor, but understand that there most likely will be a delay as there was with ICD-10, Meaningful Use, and PQRS.”
Today Clinic staff, on the other hand, are just beginning their MACRA prep. “Our plan is to continue with our quarterly provider and staff meetings where we focus on things like MACRA,” Mayer explains, adding that he too wouldn’t be surprised if the start date was pushed back.
“Honestly, I don’t know how any practice can be prepared by January 1,” Stack says. “That is why the AMA and many others are recommending that the first reporting begin no earlier than July 1. Even compiling truly useful and accurate educational material by January is a heavy lift since we don’t expect to see a final rule until sometime in October and perhaps even as late as November 1. There is nothing in the MACRA statute that sets the start date for reporting, nor is there anything in the statute mandating that the reporting period be set at a full year, so CMS should have flexibility to begin at a later date.”
No matter the start date, Stack believes that, to get off on the right MACRA foot, physicians should first assess how they are performing under current programs since the new MIPS program will be based on those. “They also should begin exploring what qualified clinical data registries are available to them,” he adds, “since this is a new reporting vehicle that could simplify processes for them as well as yield more clinically useful feedback data.”
Morris has similar suggestions, but admits that, “You’d be hard-pressed to get everything in place by January 1 unless your organization already had a lot of this stuff in place and was just tweaking around the edges. I think the analytics capabilities and understanding your costs are difficult things. Even large health systems, which spend a lot of money on those things, struggle. Measuring my quality, having the data necessary to do that, and having the information necessary to understand my costs … I would include all of those as the biggest challenges to getting started with MACRA.”
Gauging the Likelihood of MACRA Success
MACRA’s marketing problem will eventually be a thing of the past. Delayed by choice or not, the program will be here sooner rather than later and physicians will have to make up their minds as to whether participation will be done with enthusiasm, trepidation, or opted out of altogether. MACRA will soon make clear just how painful a process it is for healthcare to move from fee-for-service programs to value-based payment systems.
“Money always talks,” says Mayer, “but to be honest, I am disappointed when the focus of policy changes or the support of policy changes is dependent on the money that will be generated, saved, or lost as a result. While it is very important to consider these things carefully, I worry that we don’t consider as thoroughly the impact such changes have on patients. Despite the intention of programs like MACRA to improve the quality of patient care, it may be hard to convince physicians to participate more for that reason than to avoid fines, decreased reimbursements, or for a promised bonus. Education, support, and follow-ups will be vital, which I think CMS is good at. What I hope to avoid is the need for more support staff to understand, implement, and maintain MACRA.”
Morris puts the move to value, which one could argue started long before MACRA was introduced, in perspective: “These are baby steps. The ACA was a step. Some of the initiatives after were steps. MACRA is another step. In many ways, this is the biggest step we’ve taken so far. I think the devil will be in the details of how well it’s executed. It’s one of those things that looks good on paper. Let’s see how it really works out.”
More on MACRA: Apples, Oranges, and Start-Date Changes
Most industry insiders familiar with MACRA seemed confident that the program’s start date will be delayed. Even CMS Acting Administrator Andy Slavitt hinted at that likelihood, and has since taken steps to ease the pain of participation with start-date options. The industry’s confidence in a delay is easy to understand, given that federal regulatory delays seem to have become the norm rather than the exception. Who can forget the beleaguered roll out of ICD-10? The anticipation of a MACRA delay lends itself to a comparative look at ICD-10.
“They’re definitely in the fruit category together,” says Mitch Morris, when asked if comparing the two is akin to looking at apples or oranges. “ICD-10 was a big change that was, for the most part, not welcome and being driven by the government. That’s definitely something they have in common. As you know, ICD-10 got delayed a couple of times before it was finally implemented, but it did really require some significant changes in office practice. If done well, it shouldn’t have had a negative impact on practice income.”
Morris adds, “With MACRA, also pushed by the government, there’s no formal sign of a delay, but as we learned from ICD-10, that can change with pressure applied to the appropriate places. MACRA has the potential to really change a physician’s income up or down, particularly those in independent practice, and particularly those who have a lot of Medicare patients. It will certainly change the dynamic, especially given the requirements and infrastructure necessary to participate.”
However, Steven Stack sees no similarities whatsoever. “I think this is entirely different,” he says. “ICD-10 in many ways was a simpler issue. It was a replacement for the already existing ICD-9 mandate. The ICD-10 issue focused on the need to be more detailed in documentation providers were already doing, in training their staff, and in lack of confidence that claims would be processed in a timely manner. Physicians were being told to keep enough money in reserves to cover their payroll and office expenses for six months due to anticipated claims payment delays. Physician practices don’t normally have that kind of cash on hand, and it was very alarming.”
“MACRA is largely about modifying an already complicated Medicare physician payment system, and then adding on new requirements for those who participate in advanced payment models,” Stack says. “There are a lot of changes happening at once all across the payment system. Quality reporting and meaningful use of EHR requirements are changing. A whole new method of measuring and comparing resource use has been proposed, new clinical practice improvement activities need to be identified and documented, and so forth. This transition will be far broader and much more complicated than the move to ICD-10.”


Sounds reasonable, until you look at the Silicon Valley experience. Silicon Valley grew like a weed precisely because employees could…