I want to add the following. I'm an IT professional. In the course of my professional duties, I'm expected to…
News 3/13/15
Top News
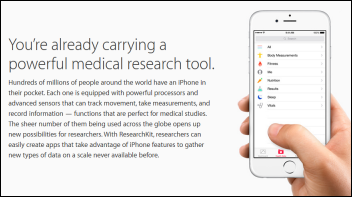
Stanford University reports that 11,000 people signed up for one of its cardiovascular studies using Apple’s ResearchKit in the first 24 hours of the app’s availability on the iPhone. The university says it usually takes a year and 50 medical centers to hit the 10,000-enrollee mark. However, the best metric won’t be known for some time and may never be announced – how many of those 11,000 casual applicants will be actually be accepted into the study and participate? My suspicion is that the majority of responses are from people screwing around with their new Apple toy who don’t realize what’s involved, so it’s going to take quite a bit of work for Stanford to get down to usable subjects. Someone make a note to ask Stanford in a month how large their cohort is and what percentage of the Apple self-submitters were accepted.
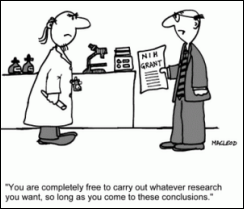
I was thinking about the “research” part of ResearchKit. Traditional medical studies involve carefully assembling a cohort of people who meet narrowly defined study criteria, with the intention of proving a specific hypothesis in a specific population. On the other hand, research using patient-generated data may uncover relationships that nobody thought of or that may prove useful in managing an individual patient’s condition even in the absence of a generalized population study. Direct care lives at the interesting intersection of big, decisive research studies and anecdotal “it just works” clinician practice based on experience. A given patient’s endless supply of non-inpatient electronic data, along with similar data generated by people like themselves, could improve that patient’s life more decisively than any study, provided that physicians are willing to practice based on data snapshots rather than studies that take many years to complete. Another positive is that studies are often funded by drug companies or special interests that have a vested interest in manipulating data in particular way or in killing a study that might hurt product sales.
Reader Comments
From Clinic Director: “Re: Meaningful Use audits. We are now at 96 audit requests of our 139 Epic-using physicians and have passed all. CMS says providers are chosen randomly, but is 70 percent of our providers really random? I needed help, so I asked our congressional office, which referred me to the auditor. ONC referred me to the CMS EHR Info line, which referred me to the auditor. The auditor referred me to the CMS Info Line. It feels as though I’ve entered the Twilight Zone.”
HIStalk Announcements and Requests
Several CMIOs expressed interest in a HIMSS get-together. I booked a table for Tuesday, April 14 at either noon or 1 p.m. right in McCormick Place and I’ll buy lunch for up to 20 attendees via the Bistro HIMSS program. CMIOs or physicians working in a CMIO-type role regardless of title can sign up here. It’s a convenient location near the exhibit hall where you can actually sit to eat (unlike most other convention center locations), the food should be decent (salads, lemon-sage chicken with polenta cakes, and dessert with healthy options), and Lorre will be on hand to say hello and introduce everybody since it was her idea.
Speaking of events, some readers are confused by the two I’m having at the HIMSS conference. Event #1: HIStalkapalooza is the big event on Monday evening – it’s open to those whom I will invite from the list of folks who previously submitted the online form indicating their desire to attend. Event #2: the sponsor-only networking event is Sunday evening and is open only to sponsors of HIStalk, HIStalk Practice, and HIStalk Connect. We’ve reached out several times to our sponsor contacts (not all of whom are efficient in passing the word along to the suits upstairs who might want to come), so Lorre will still entertain invitation requests for that event (and new sponsorship inquiries from companies anxious to talk business with their peers in a social setting). I suppose we now have Event #3: the CMIO lunch above. I just know I’m writing a lot of checks. Anyway, just to be clear, walk-ups will be politely turned away from all three events since I’m working with a fixed attendee count.

You can wear one of the four “Secret Crush” sashes like the above at HIStalkapalooza if you email me explaining why you have a crush on Dr. Jayne, Jenn, Lorre, or me. People like being sashed and I couldn’t come up with anything more original than the “Secret Crush” ones I’ve done before. I don’t expect many responses, so your odds of winning are good. Of course you need to have signed up for HIStalkapalooza and plan to attend to be sashed since I’m not mailing it for someone to wear around the house.
I’m going to stop mentioning press releases that list a hospital or health system without including its location (both city and state) because I’m annoyed at lame PR people who expect me to do their jobs in deciphering an over-edited company announcement into something factual. Surely it’s not hard to understand that “St. Mary’s Hospital” could be anywhere, as could a hospital whose location is stated only as “Missouri” (if the location is named at all). I’m also annoyed at ‘’announcements” that are too vaguely worded to tell whether a hospital has bought a new system, is beginning its implementation, or is continuing a previous installation (the latter two of which aren’t really news). Attention PR people, especially the lesser competent ones: I’ll consider running your announcement if it’s newsworthy, but being newsworthy means that you provide the five Ws: who did it, what they did, when did they did it, where it happened, and why it happened. Anybody want to see me call out exceptions?
This week on HIStalk Practice: Mental health professionals weigh the pros and cons of moving to EHRs. HealthSpot and Pacify secure new funding. LaHIE launches a patient portal. Kareo acquires DoctorBase. PatientPoint partners with Telemundo for point-of-care content. St. Peters Health Partners Medical Associates and Northwestern Memorial Physicians Group implement new population health management tools. Jim Denny digs deep into physician ICD-10 readiness.
Apple introduces ResearchKit, an open-source API designed to help medical researchers collect data from iPhone and iPad users. The Department of Homeland Security launches an accelerator program targeting wearable technology startups building applications for first responders. TechStars welcomes its second class of digital health startups to its Kansas City campus for a 12-week program. SocialWellth raises $7.5 million to expand its digital health app formulary service platform.
Webinars
March 31 (Tuesday) 1:00 ET. “Best Practices for Increasing Patient Collections.” Sponsored by MedData. Presenter: Jason Bird, director of client operations, MedData. Healthcare is perhaps the last major industry where the consumer does not generally have access to what they owe and how they can pay for their services. Collecting from patients is estimated to cost up to four times more than collecting from payers and patient pay responsibility is projected to climb to 50 percent of the healthcare dollar by the end of the decade. Learn how creating a consumer-focused culture, one that emphasizes patient satisfaction over collections, can streamline your revenue cycle process and directly impact your bottom line.
Here is the video of Thursday’s webinar by West Corporation titled “Turn Your Contact Center into a Patient-Centered Access Center.”
Acquisitions, Funding, Business, and Stock
Government contractor Maximus acquires Acentia for $300 million in cash from private equity owner Snow Phipps Group, with Maximus lustily eyeing Acentia’s contracts with HHS, FDA, NIH, CDC, CMS, and the Military Health System.
Austria-based blood sugar tracking app vendor mySugr raises $4.8 million in funding. Its FDA-approved product synchronizes data from medical devices, even using the smartphone’s camera to import readings from the displays of non-connected glucometers (that part works only in Austria).
Sales
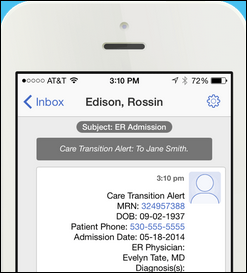
DaVita selects Cureatr for secure messaging and patient care transition event notification.
Citizens Memorial Healthcare (MO) chooses Summit Healthcare Web Services Adapter to send public health and immunization information to the state’s HIE, with plans to expand its use to meet Meaningful Use Stage 3 requirements.
Trinity Health (ND) chooses managed cybersecurity services from Leidos Health.
People

Dana Alexander (Caradigm) joins Divurgent as VP of clinical transformation.

William Bria, MD (The HCI Group) joins CHIME as EVP of medical informatics and patient safety.
Announcements and Implementations
Craneware will offer its customers analytics software from Aridhia Informatics. I’m baffled that someone thought this would be a good product name: “Aridhia Analytixagility.” It looks like the result of my snoozing off at the keyboard after working too late.
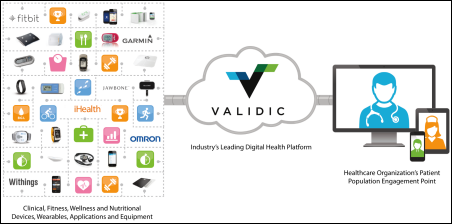
Cerner will use Validic’s digital health platform to incorporate data created by home medical devices and wearables into Cerner’s HealtheLife patient portal.
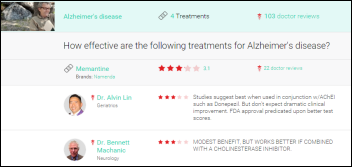
Online doctor visit service HealthTap launches RateRx, which lets its member doctors rate the effectiveness of individual drugs and treatments.
Mediware releases MediLinks Outpatient for pulmonary rehab.
Todd Fisher, who founded consulting and software engineering firm Intraprise Solutions in 1997 and was CEO of MobileMD when it was sold to Siemens in 2011, launches Intraprise Healthcare.
Government and Politics
The family of a VA patient who died of low blood oxygen levels sues the hospital after its former nurse admits turning off the patient’s alarms.
SAMHSA (HHS’s Substance Abuse and Mental Health Services Administration) launches Suicide Safe, an app that provides guidance for PCPs and behavioral health providers who are faced with potentially suicidal patients.
Privacy and Security
The US attorney indicts 11 Detroit-area residents after a former Blue Cross Blue Shield of Michigan employee provides 5,000 subscriber screen shots to accomplices who used their information to obtain phony credit cards to buy $742,000 worth of merchandise from Sam’s Club. The BCBS CEO announces new steps (the key here being that these practices weren’t already in place) that include limiting employee access to Social Security numbers, enforcing employee password changes, and installing secure printers that require employees to scan their badges before their document prints. The US Attorney makes the point that while technology makes it easier to commit identity fraud, it also makes it easier to capture those who do so. Interestingly, BCBS of Michigan brags on its site that it wasn’t part of Anthem’s breach while not featuring its own breach prominently.
Other
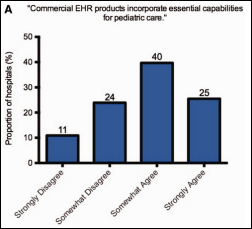
A small survey-based study of children’s hospitals finds that inpatient EHRs don’t support peds very well, adding speculation that vendor and customer fixation on Meaningful Use is delaying rollout of needed pediatric functionality. It’s somewhat of a subjective study, the survey results are old (going back to September 2011), and dumping responsibility for customer-needed features on ONC rather than the vendors selling EHRs (and thus the customers who drive their development agendas in chasing MU money) seems biased. Correlation also seems skimpy since some hospitals seem to be doing fine, presumably using the same EHR although the study didn’t ask the important question of “which product are you using and how long have you used it?” In addition, some hospitals said they weren’t interested in implementing the features that were missing, such as weight-adjusted blood pressure percentiles or immunization contraindication warnings. It would also have been helpful to know whether those that reported missing features have worse outcomes since simply having the feature available doesn’t necessarily improve care. I was going to to check the supplementary material to see how the survey was worded, but the link is dead. Quite a few publications and tweets summarized this report as thought it’s decisive and insightful, while I would say the only thing newsworthy about it (and thus why I’m mentioning it) is that it really isn’t and those writers and tweeters need to spend more time analyzing the study itself rather than dreaming up attention-seeking headlines.
Here’s a pretty funny commercial from Cox Business, tweeted out by Eric Topol, MD as an unintended reference to his new book, “The Patient Will See You Now.” He adds, “Suck it, doctor’s office.”
Ireland rolls out a national patient identifier, with the CIO of its health services saying it offers “patient safety and ensuring that the right information is associated with the right individual at the point of care. The IHI will also help in managing our health services more efficiently and ensure that health information can be shared safely, seamlessly across different healthcare organizations associated with patient care. ” The government points to effectiveness studies from Canada and the UK showing that a national ID reduces errors, improves EHR data, increases efficiency, and protects privacy.

The bond rating agency of 445-bed Memorial Hospital of Gulfport (MS) notes the hospital’s “sharp decline in liquidity in 2014” due to a Cerner EHR conversion that inflated its accounts receivable by $25 million and jumped A/R days to 100.

NBC News fires Chief Medical Editor Nancy Snyderman, MD over fallout from her previously admitted violation of voluntary 21-day Ebola quarantine when she and her crew, fresh back from Liberia, picked up takeout food. She also appeared to be impaired during a February 22 live broadcast. She will be taking a faculty position at an unnamed medical school.

Cerner’s Neal Patterson and his wife Jeanne (who has cancer) are featured in a KQED series on EHR interoperability. Jeanne says she has given up on having 20 health systems share her records with each other, so she instead carries around a bag of printouts and DVDs. Neal says, “The paradox is that I am one of the few people that should be able to fix this. I’m frustrated that we’re not moving faster.” He adds that the US is one of few countries that don’t have a national patient identifier and streamlined consent processes and that he’s putting his money where his mouth is in funding CommonWell. Epic responded to the reporter’s question of why they haven’t joined CommonWell in saying that its clients can already exchange information and Care Everywhere is “much more mature” than CommonWell. Neal says that if the industry commits to interoperability and the government creates “compelling guidelines,” the interoperability problem can be solved within 10 years.
I ran across some email exchanges between an ambulatory EHR vendor (one I’ve never heard of) and one of its practice clients. The practice, which is replacing the vendor’s system, gave its new vendor access to the old vendor’s system so they could convert patient data. The old vendor says giving them access violated its copyright and is thus a breach of contract. The old vendor is suing the practice and says it will drop the lawsuit for $25,000, adding that lack of immediate response doubles the settlement fee to $50,000. My reactions: (a) practices never seem to pay adequate attention to the contracts they sign, happily agreeing to terms that any lawyer would advise against; (b) practices also seem to choose their systems and vendors with questionable amounts of research; and (c) the old vendor has every right to hold the practice accountable for the contract it signed but shouldn’t have, although the “pay fast or we double it” part is scummy for sure. I suppose vendors are like significant others – you don’t really know what they’re capable of until you try to move on without them.
Forbes should know better than to let a private wealth advisor try to explain “How Telemedicine Can Kill You.” The lack of insight is stunning given the article’s two “potentially devastating problems”: (a) possible computer glitches that “can alter medical records” along with implantable devices “that can go haywire”; and (b) hackers. The fact that neither of these theoretical “problems” have anything specifically to do with telemedicine was missed by whoever crafted the click-baiting headline. I couldn’t decide whether to be angry at the article’s failure to deliver or to laugh at some of its unintentionally hilarious conclusions, such as “being able to control if a person lives or dies can readily lead to exhortation and murder-for-hire” (I’m assuming the author meant “extortion.”) Just last week the same editorially ubiquitous author wrote an equally lame telemedicine piece consisting entirely of quotes from a telemedicine company CEO, who not surprisingly didn’t mention killing any of his patients.
Quantros produces a video to support National Patient Safety Awareness Week, which is this week.
BIDMC CIO John Halamka, MD says that “outsourcing your mess to someone else to host is not cloud computing,” suggesting that CIOs instead focus on “Outcomes as a Service” where vendors are paid for managing people, processes, and technology.
Sponsor Updates
- Navicure completes ICD-10 testing with eight Medicare jurisdictions, to be followed by testing with all 16 jurisdictions in April.
- Nordic leads off its “HIT Breakdown” podcast series with an episode on population health and adds a new video in its series on Epic conversion planning.
- Hayes Management Consulting offers “Overcoming Resistance to Change: It’s All About the Buy-In.”
- LifeImage will exhibit at the American College of Surgeons Committee on Trauma Annual Meeting March 13 in Chicago.
- HCS will exhibit at the National Association of Psychiatric Health Systems Annual Meeting March 16-18 in Washington, DC.
- Healthfinch posts “Apps that optimize your EHR workflow are essential for care redesign.”
- IHS posts a blog on “Making the Hard Decisions” when going through the HIT selection process.
- Healthgrades gets a nod in a Forbes piece on a need for bipartisan action on healthcare transparency.
- VMware posts “Creating the Perfect Clinical Desktop with Horizon View.”
- Galen Healthcare Solutions posts the second installment of its series og on shifting to value-based payment models.
- HealthMEDX will exhibit at the LeadingAge PEAK Summit March 16-18 in Washington, D.C.
- Healthwise commemorates Patient Safety Awareness Week with “Why Safety is Personal When it Comes to Medical Care.”
- Logicworks will present at the National HIPAA Summit March 16-18 in Washington, D.C.
- Holon Solutions will exhibit at the NW Regional Critical Access Hospital Conference March 17-19 in Spokane, WA.
- Ingenious Med posts the fourteenth installment of its blog series by President and CEO Hart Williford.
- InterSystems outlines the factors creating excitement around patient engagement.
- Lifepoint Informatics will host its annual users conference March 18-19 in Orlando.
- Influence Health will exhibit at TIPAAA (the IPA Association of America) March 19-21 in San Antonio, TX.
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.



RE: We are now at 96 audit requests of our 139 Epic-using physicians and have passed all. CMS says providers are chosen randomly
The problem is that Epic is the only vendor getting it’s customers to MU in large volumes.
If only Epic customers get to MU, then even an “random” audit is going to result in mostly auditing Epic customers.
Unless of course other political interests are in play (but how could that ever happen in our fine country?).
“Attention PR people, especially the lesser competent ones: I’ll consider running your announcement if it’s newsworthy, but being newsworthy means that you provide the five Ws: who did it, what they did, when did they did it, where it happened, and why it happened.”
Don’t forget the occasional H – How.
Is Neal Patterson that naive that he can fix all the data exchange issues? Really?
I have spent my entire career in HIT both as a clinician and vendor. I’ve been carrying around my wife’s medical records in binders for years and suddenly Neal thinks he can waive his magic wand as self appoint the lord of space, time and dimension???
Here’s the gauntlet. Gather all the industry titans including Judy Faulkner and you all come to the table walking away with an iron clad and legally binding agreement that you will take the ONC standards and extend them so that every vendor can share information well beyond what ONC has mandated on the providers. Then you establish a legally binding governance structure for vendors where you will maintain, sustain and extend these efforts. Then all of you agree that you will build this in to your software, no exceptions, no excuses. Then you all agree to substantially fund this vendor driven interoperability governance body. Then you agree to work with the regulators in earnest. Then you stop lobbying Congress for your own self interest.
And do this before the federal government does as they have promised they will use every lever to force you to do.
Then you come up with a solution to the business model problem where docs are being forced to pay for sharing data needed for patient care by you and your competitors.
Stop the nonsense with CommonWell, Argonaut and any other well intended, ill begotten attempts to create consensus. Work the problem, Neal. Work the problem… Be the HIT leader you profess to be. I’m sure your shareholders will understand that this is short term loss for long term gain.
Until you do all of these things, they are just words. Empty, hollow and meaningless words.
Then you can put down your books and DVDs and society will be the better for it.
“A small survey-based study of children’s hospitals finds that inpatient EHRs don’t support peds very well…”
NIST published technical guidance on precisely that subject in 2012.
NISTIR 7865: A Human Factors Guide to Enhance EHR Usability of Critical User Interactions when Supporting Pediatric Patient Care
http://www.nist.gov/manuscript-publication-search.cfm?pub_id=911520
Pediatric patients have unique characteristics that translate into unique EHR usability challenges. It is not surprising then that the adoption of EHRs by pediatric care providers has lagged behind adoption for adult care providers. In this document, we highlight important user interactions that are especially salient for pediatric care and hence to the EHR user-centered design process. These interactions and associated usability recommendations were identified by consensus during a series of teleconferences with experts representing the disciplines of pediatrics, human factors engineering, usability, and informatics. In addition, extensive peer review was provided by experts in pediatric informatics, emergency medicine, neonatology, pediatrics, human factors engineering, usability engineering, and software development and implementation. This report details recommendations to enhance EHR usability when supporting pediatric patient care and also identifies promising areas for EHR innovation. Finally, we illustrate unique pediatric considerations in the context of representative clinical scenarios which may be helpful for formative user-centered design approaches and summative usability evaluations.