Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
News 10/21/09
From Winston Zeddemore: “Re: SNOWMED. Almost as bad as ‘HIPPA’ eruptions are ‘SNOWMED’ eruptions, where the terminologically naive misspell the name of SNOMED-CT. Here is a link to the latest, courtesy of Government Health IT.” Revisionist history does not work well with Google caches (see previous and current images above). While they were doctoring it up, they should have corrected physician’s to physicians’ unless they are being extra-pessimistic in assuming that only one doctor will be using an EMR by 2015 (not likely since they’re owned by HIMSS now). The same reporter misspelled it the same way in Government Computer News, so it’s time to fire up that spell check dictionary. Googling turns up several other examples by people who should know (or is that KNO?) better.
From Will Weider: “Re: de-identification. Wired finally picked up a story you highlighted months ago.” They sure chose odd sources in trying to flesh out a New York Times article about patient privacy: CCHIT’s marketing director, investment guy George Hill, and a 2007 quote from PAMF’s Paul Tang from Modern Healthcare (which they spelled wrong). They did, however, spell HIPAA correctly and put up a nice graphic from Patient Privacy Rights (although it was too small to read).
From ITRN: “Re: Epic. Did KLAS report they had a de-install in 2008?” I don’t have access to KLAS (I have no KLAS, in other words) so I’ll ask readers to chime in.
From DDD: “Re: Windows 7. I upgraded a month ago and have found it to be more and more intuitive every day. There’s no ‘killer app’ per se, but management of multiple apps, windows, files, etc. are amazingly different. Learn how to use it, and I’ll bet you become a fan.” They said that about Office 2007. At work, I de-installed Access 2007 and went back to 2003, every minute in front of Word is torture, and the only reason I don’t dislike Excel and PowerPoint is that I don’t use them much. Like they say, change is welcome only when the status quo is untenable, which it wasn’t. Maybe I should install Win7 on a spare PC (I love that PCs are so cheap that everyone has spares) and report.
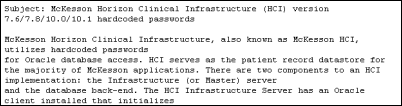
From Secret Squirrel: “Re: McKesson. Horizon Clinical Infrastructure (HCI) appears to use hard-coded database passwords. A security organization has run the entire password list online.” I thought everyone knew that, but maybe not (I reconsidered adding fuel to the technical fire, so I’m not including the link). The poster was amused that e-mailing security@mckesson.com bounced back as undeliverable. I would imagine that many vendors have services that log on as “users” that may or may not use encrypted passwords, some of which give full read/write/update database privileges. I would also imagine that vendors ship default passwords (some intended as their own “back door” in case clients screw up) that unlock every system they’ve ever sold. The clients I’ve known never seem to worry much about that.
From Just Curious: “Re: EMR. I’m sure you got this question by the thousands already, but I’m curious as to what vendor your PCP uses for his/her EMR? Thanks and keep up the great work!” It’s McKesson, he told me last time, although he didn’t seem too certain.
From Enrico Brizzi: “Re: CPHIMS. I was wondering what the industry’s current view of the CPHIMS designation is, specifically in Canada since CPHIMS-CA is fairly recent.” I have my own opinions, but I will leave others to express theirs for a change.
From Sore Arm: “Re: flu vaccine. The Atlantic is running a major article questioning the received wisdom about flu vaccines and antivirals, for both seasonal flu and H1-N1.” The article speculates that the benefit of flu vaccine has been wildly overestimated due to the inherent variability in a self-selecting patient cohort (i.e., it’s healthier people who get the shot even though unhealthy ones are the target audience, so naturally they live longer). Also, that a lot of “who the hell knows” deaths get incorrectly coded as influenza. The conclusion from a noted investigator: getting the flu shot doesn’t reduce mortality rates at all. The high-powered naysayers say, studies aside, they still believe in it and don’t like all the frowny talk. The article also questions why the US government has stockpiled millions of doses of Tamiflu and Relenza despite lack of evidence that they are effective.
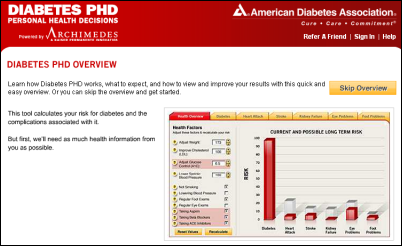
From Bernie Tupperman: “Re: Archimedes. Kaiser licenses it to corporations to screen employees, but you can use it free since it was licensed to the American Diabetes Association. You put in your numbers and it takes about 10 minutes to crunch your data to show your 30-year risk of diabetes, stroke, heart attack, and complications. You can then play with the numbers – what if you lose 20 pounds or start taking aspirin? This is a great patient motivational tool and I am busy telling EVERYONE.” That is just cool (access it here). I didn’t realize that it was Kaiser’s but it is definitely an eye-opener. Brilliant.
The VA engages the Industry Advisory Council to identify the issues involved with keeping and modernizing VistA. This sounds ominous: “… opportunities and impact of modernizing and deploying VistA upon private industry …” Surely they aren’t considering dumping VistA just to protect for-profit vendors.
Weird News Andy sniffs out this story about a high-tech scalpel that detects the presence of malignant cells from cauterization smoke, helping surgeons remove all parts of a tumor.
Gila Regional Medical Center (NM) chooses the Cboss patient payment portal.
Cleveland vendor Lakeshore Health System announces Urgicode, which notifies the pharmacy via a cellular network when a code cart is used, then allows restocking by bar code. They probably should have held off on the press release until they improved their Web site a bit, like maybe adding the company’s address, phone number, or that same press release.
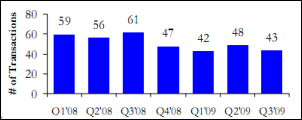
Healthcare Growth Partners releases its Q3 2009 Healthcare IT Transaction Summary (warning: PDF). Not to give away the conclusion, but merger and acquisition activity is on the upswing.
TPD forwarded a link to the Kaiser Family Foundation’s tool for comparing health care reform proposals.
I enjoy reading comments left for articles, but I need to disclose that I have the obligation to edit or remove those with advertising, personal attacks, or questionable claims. That almost never happens, but just so you know.
GE Healthcare announces that something has finally come to market from their Intermountain relationship: a new real-time decision support product. Details were skimpy and buzzwords were ample, but it might be interesting given Intermountain’s original HELP system and the work of Brent James. It will be “unveiled” at HIMSS.
Speaking of HIMSS, I keep forgetting to mention the keynote lineup for the March conference: Sprint Nextel CEO Dan Hesse (I’ve never heard of him and Sprint’s shares have dropped from $25 to $3 in four years, so I’ll pass); celebrity doctor Sanjay Gupta (you can see him free everywhere); Harry Markopolos (him I’d see – he’s the former Army officer and securities executive who tipped off the SEC boneheads about Bernie Madoff); and pilot Sully Sullenberger (who has started a safety consulting firm and might be interesting). Given the propensity of HIMSS to grab whomever is popular at the moment, I expected Balloon Boy (like Dana Carvey and that guy who sawed his own arm off in previous conferences). I should run a poll on who they should get since I haven’t been happy with the choices for several years.
Vangent, Inc. says ONCHIT has chosen its HIEOS HIE system as a component of NHIN CONNECT Gateway Version 2.2, which includes XDS.b and XCA profiles (its open source Wiki is here).
Sequel Systems announces GA of its SequelMed Patient Portal for practices, priced at $75 per provider per month according to its site.
San Francisco IPA Brown & Toland Physicians says one reason for its spat with UCSF is that the hospital didn’t want to participate in its EMR program. From Googling, it appears that the practice uses GE for practice management and Allscripts for the EMR. UCSF, you may recall, just halted its own GE Centricity Enterprise project. According to a rumor posted here last year, the IPA was threatening to cut off referrals to doctors who wanted to stop using its EMR and billing services.
More e-health fraud accusations in Canada, this time in British Columbia. Allegations have been made that health ministry officials paid falsified invoices and improperly chose vendors for an $108 million project.
And more: Canada Health Infoway is under government scrutiny for heavy use of consultants, missed deadlines, and having spent $1.6 billion so far with another $500 million on the way. The newspaper article points out that Infoway fell far short of its goal of covering 50% of Canadians with an EMR by March 2010, currently stuck at 17%. The federal auditor’s report will be out next month.
Geisinger Health System (PA) partners with Navigant Consulting to offer consulting services, including those related to EMRs and process improvement. I’m not sure how I feel about that or any other hospital business that has nothing to do with caring for their own patients, but it’s all the rage.
The managing partner of consulting firm Courtyard Group, stung hard by the reports of auditors investigating eHealth Ontario, says his firm was deeply entrenched in the project, but only because the agency’s people were clueless and without goals. He claims the company billed only $7 million of an authorized $10.6 million. His quote about the predecessor agency Smart Systems, which spent $800 million to build a non-Internet based network that went mostly unused: “I remember a conversation with the previous CEO of Smart Systems and he was very proud of the fact Ontario was the only jurisdiction in the world building a private health network. My reaction was, maybe the fact we are the only ones doing it might be an indication this is a bad idea.”
Epocrates announces that its drug reference will run on BlackBerrys.
Virtual Radiologic upgrades its vRad Enterprise Connect product work with new mobile device and speech recognition support.
Cedars-Sinai and GE Healthcare get their first lawsuit (of many, no doubt, and this one seeks class action status) over the CT radiation overdoses caused by unnoticed equipment settings.
Odd: the IT guy at an animal hospital changes the computer system to record a Valium tablet dispense when artificial tears were ordered, allowing him to pocket 18 of the tablets worth $3. The animal hospital let him slide after he quit over it, but then filed a report after the admitted addict tried to claim unemployment.
MIT’s Technology Review interviews ONCHIT head David Blumenthal. I like his terse answers: the writer asked why insurance companies don’t push EMRs, and he said, “The insurance companies have been able to pass along the costs of waste in our health-care system to their clients.” When asked about why progressive hospitals like Blumenthal’s own Mass General don’t share data, he said, “There has never been a business case for health-information exchange. As a matter of fact, there has been a negative case: if you give away your information, you may lose it. You may lose the patient.”
HERtalk by Inga
California-based St. Joseph Health System cancels its Perot IT outsourcing contract and establishes a new system-wide service center in Lubbock, TX, expecting to add 60 jobs and $3.1 million in salaries the first year.
Healthcare deals represented nearly 30% of all US mergers so far this year, based on dollar value. Typically, healthcare represents only 10%.
Swedish company Anoto Group announces that the EDs at Western Maryland Health System have transitioned to MEDITECH’s EMR and are using Anoto’s digital pen and paper technology. In case you missed it, I mentioned a similar product called Shareable Ink that I saw at last week’s MGMA meeting. As long as the data capture will fully integrates with the EHR and the price point is reasonable, I think the digital pen technology has a lot of potential.
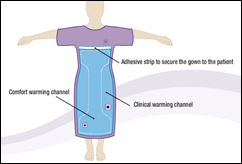
I’m thinking about trading out my Snuggie for one of these. Arizant Healthcare introduces a fully covered hospital gown that features a built-in warming system that blows warm air through tiny holes in the garment. The “Bair Paws Flex” gown sounds like the perfect Christmas gift for that hard-to-buy-for relative.
Cerner teams up with CDW to promote Cerner’s PowerWorks, the first time Cerner has offered its ambulatory suite through a national partner. Clearly Cerner wants to make sure it receives its share of the ambulatory EHR money that vendors expect to flood the market.
Picis announces that 25 hospitals have selected its Anesthesia Manager software this year. Among the new contracts are two with the VA for Picis Anesthesia Manager, PACU Manager, and Critical Care Manager.
University Children’s Eye Center (NJ) selects SRS’s hybrid EMR product. The Eye Center’s physicians are on faculty at RWJU and St. Peter’s University Hospital.
Axolotl Corp. realigns its management team, naming a new president, COO, and two VPs.
Wolters Kluwer Health announces new sales, including SwedishAmerican Health System’s (IL) and Signature Healthcare Brockton Hospital’s (MA) purchase of ProVation Order Sets to automate authoring and maintenance of evidence-based order sets. Sadler Clinic (TX) is also adding ProVation MD for procedure documentation and coding.
Oregon Health & Science University says it has received $51.5 million in ARRA funding, which has helped create 116 full- and part-time jobs. That’s about $444,000 a job, though the university does expect to add more. So far, the grants have funded over 100 research projects which require additional lab employees.
Eclipsys names six winners in its 2009 Circle of Excellence Awards. Winners had to demonstrate innovation and achievements in process improvement, adoption, or collaboration, or actively participate in the Eclipsys ClientConnect program. Recipients were given $2,000 to be donated to a charity of their choice.
Rutland Regional Medical Center (VT) agrees to serve as a national host site for visiting community hospitals. Rutland will demonstrate to visiting clinicians and administrators how they utilize various GE solutions.
The MEDSEEK folks informed us of their ranking in Deloitte’s Technology Fast 500 program, based on the company’s 346% fiscal year revenue growth over the past five years. There was no healthcare-specific grouping. but I identified several in the “software” group. Congrats to GetWellNetwork, CAREfx, Red Hat, CodeRyte, athenahealth, and other HIT companies making the list.
BryanLGH Medical Center (NE) contracts for Salar’s electronic forms tool.
NorthBay Healthcare (CA) retains PHNS to assess its readiness for obtaining ARRA funding, an example of stimulating the economy without the government spending a dime.
Physicians are using Kryptiq’s escriptMessenger software to send 310% more electronic prescriptions than last year. Its 10,000 users send about 1 million electronic prescriptions per month. I think it is safe to say that e-prescribing is finally catching on, in the same way everyone has long been predicting EMR will. Hard to believe it has been 5-1/2 years since George W. Bush made mention of computerized health records in his 2004 State of the Union address.
Social media update: I now have 25 friends on Facebook (and frankly pretty amused by the amount of time some of our readers spend doing goofy quizzes). Also, 216 connections in LinkedIn (which is about 100 less than Mr. H, but who is counting?) Also, 574 followers on Twitter (200 less than Mr. H, not that I noticed.) Forever the undercard.






What’s Wired saying about the Flu business?
Cover Story: An Epidemic of Fear: How Panicked Parents Skipping Shots Endangers Us All
http://www.wired.com/magazine/2009/10/ff_waronscience/
The MisInformants: Prominent Voices in the AntiVaccine Crusade (list includes Jenny McCarthy, Jim Carrey, Joe Lieberman, Don Imus, and MSNBC’s Joe Scarborough)
http://www.wired.com/magazine/2009/10/ff_waronscience_misinformants
What’s the Real Story on the Vaccine Debate. Learn More (calls out disguised anti-vaccine websites, and provides links to reputable information on CDC and NIH websites)
http://www.wired.com/magazine/2009/10/ff_waronscience_reading
How to Win an Argument About Vaccines (sets out myths and facts)
http://www.wired.com/magazine/2009/10/ff_waronscience_argument
Dr. Blumenthal offers negative justification for the $ 50 billion from taxpayers. Wow, he said that several years ago, he learned that a patient had an allergy to sulfa when he entered bactrim on his CPOE machine. If he spoke with the patient, he would have known that also. He implies that the CPOE machine saved the patient’s life (or did it only prevent a rash?). $50 Billion for that?
Users report that this equipment might help in simple cases, but seriously interferes with the care of complex patients.
Blumenthal has not any proof for his statements waxing on the benefits, that ignore the issue of proven safety.
Suzie, RN, have you seen this?
The Story of the Deployment of an ED Clinical Information
System ‐ Systemic Failure or Bad Luck?
http://www.it.usyd.edu.au/%7Ehitru/index.php?option=com_content&task=view&id=91&Itemid=146 , click on item #6.
From the report above;
“Hence, this study is not built on a systemic canvas
of a considered set of opinions nor experiences.”
It’s not a study, but a collection of quotes from a self selected group of unhappy users, much like the comments section on HISTalk.
Many of the issues were with it being an Australian health group using a system written for American workflows.
One ER in Wales deinstalled the device because it was endangering patients. There is not need for study when the device causes mayhem. It is not fit for purpose. The story replays in the UK and in the US. Doctors are punished for reporting the truth.
Regarding Brown & Toland Medical Group pushing UCSF doctors out, this EMR business is nothing but a red herring. Some 160,000 HMO patients will lose unrestricted access to world-class UCSF specialists all because CPMC wanted to monopolize referrals for its own doctors. Dr. Joel Klompus, B&T board chairman, belongs to the same practice group as Dr. Martin Brotman, former CPMC CEO and current Sutter Health West Bay Region president, and Dr. Damian Augustyn, chief of CPMC’s medical staff. It’s the good ol’ boy network run amok and HMO patients are caught in the middle!
Harvard’s Blumenthal Sts: ” I still think that on the whole, across the country we’d be better off with universal availability of electronic health records. We’d have fewer errors, fewer missed diagnoses, less duplication of tests, and fewer adverse drug events.”
Before spending our money, Dr. B, where is the evidence that supports your statements? At best, the error rates and adverse events will be a wash. Was it not Harvard’s research arm that was influenced by the hype from HIMSS and CCHIT?
Harvard’s Blumenthal Sts: ” I still think that on the whole, across the country we’d be better off with universal availability of electronic health records. We’d have fewer errors, fewer missed diagnoses, less duplication of tests, and fewer adverse drug events.”
Before spending our money, Dr. B, where is the evidence that supports your statements? At best, the error rates and adverse events will be a wash. Was it not Harvard’s research arm that was influenced by the hype from HIMSS and CCHIT?
blah wrote:
“Many of the issues were with it being an Australian health group using a system written for American workflows.”
Written by … whom?
Most graduates of even an introductory course in healthcare informatics recognize the need to adapt IT to the culture in which it will be used – and well before implementation.
Neil, if you read this blog, can you please comment? Did Cerner perform that analysis and modification, or not? If not, why not?
Mr. HIStalk, your comments about HIMSS’ conference lineup made me laugh!! Perhaps you should create a poll. The results would be very interesting and provide guidance to HIMSS.
Keeping in line with HIMSS’ expansion of conference seminars for ARRA, perhaps it would not be a bad idea to hire Mark Leavitt, CCHIT chair, as a keynote speaker. Leavitt appears to have entered the fortune teller business. It would be fun to see Leavitt consult his crystal ball and/or tea leaves in real time! I would pay extra to see that.
http://www.healthcareitnews.com/blog/cchits-latest-gambit
MedInformaticsMD i agree 100%, thats the way it should work. Just pointing out the flaws in the “study”.
Blah,
OK.
Just want to mention that the new AHIMA/AMIA book “H.I.T. or Miss: Lessons Learned from Health Information Technology Implementations” is due out in November. It contains information that should be of use to the audience here.
I was an associate editor along with a group of other medical informatics specialists who have led successful electronic health record (EHR) and Health Information Technology (HIT) projects.
See https://imis.ahima.org/orders/productDetail.cfm?pc=AB102209&bURL=%2Forders%2Findex.cfm%3F
Note: we will not be getting royalties on the book.
blah would like to dismiss my study of the deployment of Firstnet in Australia as “a collection of quotes from a self selected group of unhappy users”. Thank you for pointing out my oversight in describing the commentator group which included clinicians, administrators, and an ex-Cerner employee. I have added a sentence to the essay to correct that defect.
If he had read the article or even paid attention to the title it is presented as a “critical essay”, that is, it presents an analysis of what the users find wrong with the system ( the collection of quotes) and then assesses what other factors are contributing to the failures in the roll-out, such as the refusal of some hospitals to accept it in the first place and others to discontinue using it within days of roll out. These included discussion of the contract and its fulfilment.
You comment “Many of the issues were with it being an Australian health group using a system written for American workflows” is entirely unrepresentative of the article which only mentions this factor as one of the issues.
A closer reading of the article would make you more informed to comment.
Contrary
Apophis posted an important link. I was not aware of it.
It generated healthy discussion.
Users with whom I speak use similar language to describe experiences with CPOE and electronic medical data storage devices.
The HIT industry has neither transparency nor accountability.
We need to escalate the issues. Bring them to the attention of NIST and the FDA. Report adverse events and errors. Write and post.
If the industry had to answer to the FDA, there would be a shift to fixing the problems that have been known for years.
Jon,
Your essay raises several questions.
When I was a CMIO at a 1400+ bed hospital system a decade ago, a regional center in a state with very few hospitals at all (Delaware), I counseled that the best solution in my opinion for the very, very busy ED was document imaging of paper, supplemented by a nurse/intake triage system to rapidly record and/or confirm basics (e.g., meds/major problems/allergies/vitals) that was interfaced to the main EHR system.
I based this on the assessment that in the ED, a localized and “closed” environment, the incidence of charts getting lost or writing being illegible resulting in adverse outcomes was minimal. Charts also did not get lost when patients moved to the floors and were adequate for quick transfer and acceptance. Therefore we felt images of past ED charts (of paper) would be satisfactory for assisting care in the ED, where time constraints and hectic pace made the type of system you describe disadvantageous (and for exactly the reasons you describe in your essay).
Document imaging is a proven technology that works well even in high volume settings. For example I managed a departmental budget of $13 million, as did an entire pharma company, using an enterprise document imaging system.
I’ve also been startled by the ED EHR installed at the hospital where I take my mother, who unfortunately has needed far too many admissions in recent years than I care to see. Some of the ED staff were my former medical colleagues and even high school classmates. They’ve told me, in no uncertain terms, that the system is terrible, again for many of the reasons you cite. My own views of it (albeit brief) showed what appeared to be a mission hostile environment, including multiple very tiny pulldowns, picklists, and screens. Most recently that system did not prevent busy ED docs from almost giving my mother Levaquin after her telling the triage nurse it had caused tendon rupture in the past – and the data being entered. They actually brought in a bag of it to hang, and if I’d not been there as medical advocate for my mother they might have given it. Then when she got to the floor, the next day they almost gave it to her again, except by this time mom was her own medical
advocate. I trained in that hospital, Abington Memorial, and as Admitting Officer to the ED held the record for the most number of admissions, ever, in one night (New Year’s Eve 1986), when it was beyond crazy, starting out with one of our own physicians being brought in, shot in the chest, and dying after open heart massage just to set the mood. We managed on paper, and despite out gloomy emotional state not a single error occurred, to my knowledge.
With all this in mind:
Do we really need full EHR’s in the ED?
Is there literature that shows that the time, expense, and resources for a full ED EHR are worth it in terms of clinical outcomes, ROI etc.?
Or are we over-computerizing healthcare, even environments where doing so might actuallyube deleterious due to the nature of the environment, just because “we can” (and because there is money to be made by some)?
By the way, guess who got to do the open heart massage on our colleague? The surgeons cut; the lowly Medical Admission Officer gets to do the massage.
Honestly, did HIT create errors or just uncover faulty workflow processes? How many errors were user created within the system? HIT systems have literally, in almost all cases, been slid into a paper-based workflow environment & made to adapt to that workflow instead of creating a different workflow that made more sense with the IT solution. They are usually used alongside with paper processes still in place (i.e. documentation, med orders, etc.). While still in it’s infancy of development and use with the majority of clinicians in the US, HIT has FAR more advantages than a paper-based system could have ever produced. The transference of knowledge with the ability of sharing the patient record between the physician practice to the inpatient setting, disease management & trending for research, and the ability to develop standard best practices for care plans is monumental. I have yet to find a physician who doesn’t agree that the current paper-based system they are in meets zero of those extremely important needs.
At the end of the day, this isn’t going away (HIT) and instead of being a force of resistance, use your knowledge to help better the solutions. I also find it incredibly difficult to understand an un-automated ED works more efficiently all-around than an automated ED. While I don’t have the studies on hand (but have seen them), if anyone would be so kind to link the ample amounts of studies where it has shown that an ED has been able to increase volume, have better reimbursements, cut down on errors, and have had more time to spend with patients & providing care. I think some of the pitfalls is that many EDs are resistant to changing their outdated workflow processes to streamline and take advantage of the systems in which they purchased. Instead, they insist on keeping the redundant processes that were set in place for their paper environment. Remind me again of how long it takes to pull a paper record from Medical Records vs. one within an EMR?
Pezman, your comments are accurate in terms of replacing a paper file with an electronic file for accessibility to the contents of the file. However to accept that HIT is good because it has done its job at that point is to be complacent.
The NSW Case study has amongst, other things, two circumstances relevant to your comments. Firstly, there are EDs with an existing clinical information system and lots of experience in HIT. They found that their data entry costs/time had significantly increased relative to their old system. The only gain they got compared to the old system was better patient tracking (in my report the one of two persons who supported FirstNet did so because he wanted the tracking and he told others they expected too much by trying to use it for patient notes). The losses were: time, which caused them to drop the data entry for patient notes where they reverted to paper records after years of electronic records, (as a researcher who specialises in natural language processing I’m sure you could hear me cry); and 50% decrease in the number of patients seen by a doctor within 20 minutes of arriving at ED.
The second circumstance is the smaller rural hospital with no previous IT. They would seem to fit your scenario precisely, however there are two unexpected components in this case. More than 80% of GPs in Australia have clinical information systems in their private practices, and these are the people who staff rural hospitals. So they are well experienced to assess new systems. The most IT expert of these GPs have built their own systems, which is the situation in question for the most expressive case I quoted in my report. They ran systematic tests on using Firstnet for data entry and found that it cost them 30% more time to do their data capture. They argued that this result had an interesting multiplier effect in that the NSWHealth would have to pay them 30% more for each patient to maintain their income level, but that the department would then have to pay another 30% for the patients they couldn’t now attend to because of their increased time with the other patients. That’s a 60% cost increase. The second element of their problem with Firstnet was that in rural hospitals staffing levels are minimalist and that nurses worked with heavily multi-tasked responsibilities. Their complaint is that these staff could not afford to be used for increased data entry as it would take their attention away from the critical care issues they had to attend to that were all around them – this is a patient safety issue.
Finally my point is that IT has be efficient and applied wisely in health contexts for it to provide the gains people expect of it. We haven’t been shown yet that has been achieved in the NSW case and many believe we will be waiting a long time if at all to hear it.
cheers
jon
MedInformaticsMD introduces many good questions about the nature and role of EMR in the ED, however I don’t really know what an EMR is; how extensive is it, where does it get its data from, etc.. I think there is a clear case for the use of a clinical information system (CIS). However i also think it needs to be defined in ways that facilitate the workflow of the respective ED where it is installed. This “personalisation” is critical to a very successful CIS implementation, but the challenge is how to create such a system. Our own research is focused on creating a Generative Clinical Information Management System (GCIMS) (some details at http://www.it.usyd.edu.au/~hitru) where the notion is that the clinician specifies exactly what they want and our system generates that system. More importantly they can change it at any on their own initiative day or night and have the new version immediately available. We are currently building two pilot systems for Trauma, and Geriatric/Stroke/General Med Ward.
A GCIMS-ED system would allow clinical staff to create a system as lightweight as needed to do their tasks and tailor it at any time. The Trauma system is a good example where its first design followed exactly the forms they had developed to streamline their process. Once we did a usability test they made a significant re-organisation of their forms. That required no change from our side just a re-jigging of their specifications.
So my answer to the question is that you have to provide for a system designed by the users for the users and changeable at any time by the users, then they will get what they need and the ED will increase productivity and patient care and safety. How we do that – we’re working on it.
cheers
jon