Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…
Readers Write 12/4/08
Submit your article of up to 500 words in length, subject to editing for clarity and brevity. Use your real or phony name (your choice – we’ll substitute a phony one unless you ask specifically to be named). Submissions are subject to approval and become the property of HIStalk.
Low Cost IT Hospital Improvement Project
By Leonard Kravitz, Informatics Director 
We gave Blackberrys to all members our interdisciplinary ICU team — physicians, nurses, social work, pharmacy, dietician, etc. It was a total of 39 devices. Most staff sign up for a device when they start their shift, although some have their own device (like the ICU director and physicians). These are text-only, no voice.
They provided a huge improvement in communication efficiency. There was no more wasted time trying to find the physician or nursing trying to find pharmacy about a missing med. The bottom line is faster, more efficient care for patients and reduced errors.
The total cost is around $17K. The only reason it is that much is because we are running the devices over a cell network. We will be moving to VoIP over Wi-Fi in the next year and costs should fall to $5K/year.
What is good about this is that it’s technology that works and makes a big difference. Text-only is not disruptive, it has a time-stamped, legible message, it can be sent to many people at once, and the pagers can receive alerts from our clinical system.
The key to success is giving devices to everyone on the team, which increases the value of the network.
Low Cost IT Hospital Improvement Project
By Larry Spannel, Hospital CIO
We discovered a significant opportunity to improve customer service for our nursing and clinical staff. Like everyone else, if a problem occurred with their computer equipment, the nursing staff was expected to call the Help Desk and arrange for service. We found that this rarely happened.
When a nurse or physician had a problem with a workstation, they would leave it and find one that worked. They never had time to call and report the broken device. It was not unusual for a nursing unit to have a large number of its workstations out of service before IT was aware of the problem. In our heavily automated clinical environment, this was a real concern.
We asked our Help Desk and Field Services staff to think of a better way to ensure that all of our nursing unit workstations were available all of the time. They developed an equipment rounding plan where our field services techs visit every nursing station, every weekday. The techs inspect every workstation and printer, and fix any problems they find.
We piloted the rounding program for a couple of weeks to see if it would be effective. We were amazed at the reception we received from the clinical staff. They loved the fact that they did not have to worry about equipment availability anymore, and that they were no longer tied up making calls to the Help Desk. Where once our clinicians had a very low regard for IT support, the techs are now welcomed and appreciated for their work.
The program was so successful that we quickly implemented it for our emergency department and all of our nursing units. The program is cited as an example of excellent customer service throughout the hospital. It was a zero-cost change since we rearranged the work of our existing staff to do the rounding.
The Impact of Technology on Diabetes
By Marc Winchester, President
Digital Healthcare Inc.
Diabetes is a pervasive chronic disease that affects the coronary, neurological, renal and vision systems of over 22 million Americans with an additional 50 million termed as "pre-diabetic". If left untreated, it will remain the leading cause of lower limb amputations, end stage kidney failure, and blindness in the working age population. In terms of economic impact, the disease has no equal. Conservative estimates indicate that the annual cost of diabetes is now well over $100 million.
Technology has a critical part to play in the assessment of risk, diagnosis, treatment, and management of the disease. In order to manage the condition, technology needs to be pervasive across the care continuum.
It may surprise some to learn that diabetes can be prevented and, in the early stages, it can be reversed. This requires lifestyle change and increased awareness among the high risk population group. The role of technology in the first instance is one of supporting public health communications. Patients need to have access to simple risk calculators that can predict early onset; Personal Health records need to be easy to use and easily accessible. However, it is important to realize that those at most risk tend to also be the most technology-averse. Until this issue is addressed, technology won’t have an impact on the care process until after a patient’s initial diagnosis.
When a patient presents to the primary care physician with diabetic symptoms, a series of tests is performed to confirm diagnosis. Most medical record systems are more than capable of storing the information. However medical record systems must identify those at risk through general health, genetic, and lifestyle data. A real advantage would be a system that assesses risk and red flags patients before they have full-blown diabetes.
As the disease progresses, physicians are left with a series of options to arrest its progress through pharmacological intervention, lifestyle advice, and ultimately, referral to secondary specialists, such as endocrinologists or ophthalmologists. Efficient referrals must aim to manage the patient through a defined "care pathway," but patients rarely comply with such instructions. Technology should integrate contact management systems to ensure that patients are "nagged" by whatever means to follow up on their prescribed care plan.
In order for technology to have a real impact on chronic conditions, it must integrate diverse components into a workflow similar to that used in manufacturing processes. At Digital Healthcare, we have found the way to achieve this is to place detection technology in the primary care setting and have an automated pathway send high resolution images and data to a clinical specialist. The specialist systematically assesses the risk and recommends the next treatment option, which is also defined in the pathway. So far, we have saved the sight of thousands of people around the world using this approach.
Until we see the convergence of technology with public health policy, evidence-based medicine, and uniform reimbursement strategies, simple disconnects will continue to contribute to many more deaths and the continuing rise in health insurance premiums.
Clinical Software Review - Microsoft CUI – Secondary Care
By The PACS Designer
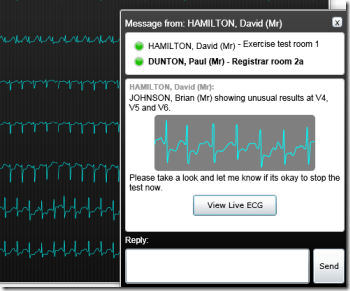
The Microsoft Common User Interface has been released for review and user input based on Microsoft’s Silverlight platform. We will be reviewing Secondary Care for Brian Johnson.
To proceed with this lesson you need to have Microsoft’s Silverlight platform installed on your system.
We are going to launch the Patient Journey Demonstration. Once you are on the Patient Journey Demonstration page, you are going to be navigating to the Secondary Care section, so click the "Launch Button" under "Secondary Care". Follow the steps below to learn the best method for navigating:
- Brian Johnson has been sent to the ECG Laboratory for a stress test. Brian is in Exercise Test Room One. While waiting for a message to appear on your screen, click "Molecule triggers allergy attack" in the "Health News box" to view the article, then close it. When the message pops up for viewing his test results, click the "View LIVE ECG" button in the message.
- Next, you will see Brian’s ECG images. The message requested that you look at V4, V5, and V6. Click the down arrow to the right of "Select a lead" then click "V4" to view the ECG image.
- Next, click the "white box" below "V4" to view "V5". Then click "white box" again below "V5" to view "V6". When done, click "V6" to return to all ECG images.
- At the left under "Chest Pain Clinic" click Brian Johnson’s "View Results" to see the data.
- Move your pointer over "Stage 4" that is on your extreme left and click the "Red Box" in the upper right corner to expand it. Next, move your pointer up to the numbers " 0 thru S" in the upper right of the screen and click the second "Red 4". Again, click the small "Red Box" to expand it and when done viewing it click again to return.
- Next, click "Known Allergies" to see Brian’s allergies. When you are done, click the "Up Arrow" to the right to close.
- Click "Search Care Pathway Library" in the lower right hand corner, then click "Angiogram/Angioplasty" to see other aspects of Brian’s health record.
- At the bottom of the screen, click "Review results" in box marked "Angiogram" to see Brian’s angiogram. Click the "Play Button" to run the viewer. Next, on the left side of screen under "Select Run," click the down arrow and then click "LAO 30 Cranial 26" to view the 3D image, then use your pointer to move the 3D to the left and right for slower viewing.
- For the last step in this review, click the "Show Guide" in the upper right corner to view all the capabilities of the online viewer. The "Show Guide" can be accessed for each viewing screen for more information by clicking "1. Registrar landing page" through "5. Angiogram" for this Microsoft CUI. Close "Show Guide" when done.
This completes the third and last review of the Microsoft Common User Interface (previous lessons are here and here). Please let us know your feelings about this new concept from Microsoft.



Just be careful where you are running “Silverlight”
(From many Microsoft license agreements:)
Not intended for use in machinery, medical or industrial applications.
I am curious about the rounding article. How big an organization this is? How many workstations, printer and locations they have. Also if they had to increase the number of staff.
[From Mr. HIStalk] I looked the hospital up and it’s in the 800-bed range. They did not increase staff, according to the CIO. We did something similar at one of my hospitals (500-bed range), assigning field techs to units for weekly or so visits. No staff increase there and the techs loved getting out to work with users in a more proactive way. If nothing else, they would clean the printers knowing we’d get called for that eventually anyway. Often they would find bigger problems with security or application problems just by being out on the front lines. This might be one of those “IT Department Marketing” projects!